Peanut allergy is the most common food allergy in children and that number has been rising – peanut allergy incidence increased 21 percent from 2010 to 2017. Almost 2.5 percent of children in the US are thought to have a peanut allergy, according to the American College of Allergy, Asthma, and Immunology (ACAAI).
Imagine not being able to enjoy a peanut butter and jelly sandwich (or even be around people who are eating one). That is one of many concerns that the estimated 1.2 million American children and teens with a peanut allergy have daily.
Peanut allergy is the most common food allergy in children and that number has been rising – peanut allergy incidence increased 21 percent from 2010 to 2017. Almost 2.5 percent of children in the US are thought to have a peanut allergy, according to the American College of Allergy, Asthma, and Immunology (ACAAI).
Despite it being a relatively common problem, there is no cure for peanut allergy. So, what is being done to develop treatments? First, let’s review what we know about peanut allergy and how we currently manage it.
What’s included?
- Overview
- Current treatments
- Drug pipeline
- Phase 3 Clinical Trials
- Phase 2 Clinical Trials
- Early-stage drug highlights
- Outlook
Peanut allergy overview
Allergies occur when your body’s immune system overreacts to an otherwise innocuous substance, in this case, peanut protein. Although some children may grow out of their peanut allergy, most do not. Therefore, peanut allergy is likely a lifelong affliction that can cause severe allergic reactions upon accidental exposure to peanuts.
Peanut allergy has become infamous for being the leading cause of food allergy-linked death due to anaphylaxis, a very severe, sudden-onset side effect of allergies that requires immediate medical attention and can be fatal. Anaphylaxis symptoms include impaired breathing, throat swelling, sudden blood pressure drop, pale skin, blue lips, dizziness, and fainting. However, an allergic reaction to peanuts may include various other non-fatal (but still unpleasant) symptoms, including indigestion, stomach cramps, vomiting, diarrhea, wheezing, shortness of breath, cough, hives, tongue/lip swelling, or confusion.
Peanut allergy is diagnosed both by empirical data, such as keeping a food diary of any reactions and trying an elimination diet, and lab testing, such as a skin test or blood test. There are three types of allergy skin tests: the skin prick test, where the skin is pricked so the allergen goes under the skin’s surface; the intradermal skin test, where the allergen is injected right below the skin’s surface; and patch testing, where a patch containing the allergen is taped to the skin for 48 hours. The blood test measures the levels of peanut-specific immunoglobulin E (IgE), with increasing levels corresponding to the increasing likelihood of peanut allergy. However, a positive skin test doesn’t always mean the patient has a peanut allergy and a negative blood IgE test doesn’t rule out a peanut allergy.
To confirm a peanut allergy diagnosis, an oral food challenge, where one ingests small and increasing amounts of peanut under the close watch of medical professionals, can be used. Although they run the risk of inducing severe allergic reactions or anaphylaxis, oral food challenges are generally safe because they are performed under medical supervision with rescue medication, such as epinephrine, readily available. These tests can also provide peace of mind, either way, to confirm or rule out a peanut allergy diagnosis.
Current treatments
Historically, peanut avoidance was considered the first line of treatment for anyone at risk of developing a peanut allergy. However, the National Institute of Allergy and Infectious Diseases (NIAID) completely reversed their recommendations for children at risk of peanut allergy in 2017 after the Learning Early About Peanut allergy (LEAP) trial showed that children at high risk for having peanut allergy were less likely to develop an allergy if they were exposed to peanuts within their first 12 months of life. Of the infants at high risk of developing a peanut allergy, only 1.9 percent who were introduced to peanuts early on developed a peanut allergy by age 5 compared to 13.7 percent who avoided peanuts. This provided hope that peanut allergies may actually be prevented by exposing children to peanuts early enough if they haven’t yet developed a peanut allergy.
The updated guidelines outlined when children should be introduced to peanuts based on their allergy risk: high-risk children (with severe eczema, egg allergy, or both) around 4-6 months, moderate-risk children (with mild-to-moderate eczema or other food allergies) around 6 months, and low-risk children (without eczema or food allergies) at their parent’s discretion. High-risk children should be tested for peanut allergy by an allergist before introducing them to peanuts to ensure they aren’t already allergic.
For people who already have a peanut allergy, avoidance is still advised. Patients should also carry a rescue medication, such as an epinephrine injector (the EpiPen, among other brands), at all times in case of accidental exposure. Antihistamines, such as diphenhydramine (Benadryl), may also be used to treat milder allergic reaction symptoms after peanut exposure.
There is no cure for peanut allergy, but there are drugs in development to reduce the severity of symptoms upon exposure to peanuts, allowing patients to potentially avoid severe reactions and anaphylaxis after accidental peanut exposure.
Drug pipeline
The allergy drug pipeline got a boost in funding during the past few years, especially for drugs that alter the course of allergies and prevent allergic reactions from starting, not just controlling symptoms once they start. This boost has helped bring drug candidates through clinical trials: as of October 30, 2019, a non-exhaustive search using the keywords “peanut allergy” on ClinicalTrials.gov gave 144 clinical trial results.
There are no FDA-approved drugs currently, but the top drug candidates are vying for FDA approval in early 2020. Here’s an overview of the major drugs in the pipeline for peanut allergy.
Note: This is not meant to be an exhaustive list of drugs in development, but a summary of later-stage and some interesting early-stage drugs in the pipeline.
Phase 3
Palforzia (AR101) [Aimmune Therapeutics] – oral immunotherapy (OIT)
Palforzia, formerly called AR101, is a biologic oral immunotherapy that trains the patient’s immune system to become desensitized to peanuts over time. This isn’t a traditional drug – it’s essentially carefully measured defatted protein flour in specific doses that patients can add to their food. The powder is portioned to deliver exact amounts of peanut protein, building up to a maintenance dose of 300 mg (corresponding to about one peanut kernel).
Patients first undergo a dose escalation period where they add Palforzia to food and gradually increase the dose they ingest over about a 6-month period. Patients then enter the maintenance period where they continue taking a therapeutic dose of Palforzia daily.
Aimmune’s Phase 3 trial, Peanut Allergy Oral Immunotherapy Study of AR101 for Desensitization in Children and Adults (PALISADE), studied how effectively Palforzia improved peanut tolerance in peanut-allergic people ages 4-55. The largest effect was seen in children and teens ages 4-17: 67 percent of participants (250 of 372) who received Palforzia could ingest 600 mg or more of protein powder (about 2 peanut kernels) without moderate to severe symptoms, compared to only 4 percent of participants (5 of 124) who received placebo. Only 10 percent of participants ages 4-17 who received Palforzia needed to use rescue epinephrine for their symptoms during the food challenge at the end of the maintenance period, compared to 53 percent who received a placebo. The lack of efficacy seen in adults ages 18-55 could be due to small sample sizes (only 41 participants received Palforzia and 14 received placebo).
The major downside to oral immunotherapy is its ability to increase the risk of anaphylaxis. This shouldn’t be surprising – if you’re ingesting the food you’re allergic too, even in small and controlled doses, you would expect to have some side effects, especially when you start scaling up the doses to induce desensitization to the allergen. Palforzia doesn’t seem to be an exception: more than 95 percent of participants ages 4-17 who received either Palforzia or placebo had an adverse event during the intervention period.
This increased risk of side effects largely accounts for the noticeably high number of patients that withdrew during the study: 22 percent of participants ages 4-17 (80 of 372) and 54 percent of participants ages 18-55 (22 of 41) who received Palforzia withdrew from the study, compared to 8 percent of participants ages 4-17 (10 of 124) and 7 percent of participants ages 18-55 (1 of 14) who received placebo.
An open-label roll-over study from PALISADE (ARC004) showed that an additional 28 weeks of daily Palforzia maintenance dosing increased the patients’ ability to tolerate higher concentrations of peanut. Eighty percent of patients could tolerate 1,000 mg of peanut protein (about 3-4 peanut kernels) and 49 percent could tolerate the highest dose of 2,000 mg (about 6-7 peanut kernels). This shows the sustained efficacy of Palforzia and that there were less adverse events as dosing continues, likely due to the increased desensitization.
Aimmune has additional Phase 3 trials, including the Real-World AR101 Market Supporting Experience Study in Peanut-Allergic Children (RAMSES) to evaluate the safety and efficacy of Palforzia in children ages 4-17 without requiring an initial food challenge, and AR101 Trial in Europe Measuring Oral Immunotherapy Success (ARTEMIS) to study the safety and efficacy of Palforzia in children ages 4-17 at various trial sites in Europe.
Despite the risk of side effects, Palforzia is still highly effective at desensitizing people with peanut allergy, ultimately allowing them to prevent major allergic reactions in case of accidental peanut ingestion. Palforzia received FDA Fast Track Designation in 2014 and Breakthrough Designation in 2015. In March 2019, the FDA accepted Palforzia’s Biologics License Application (BLA) and aims to review it by late January 2020. Most recently in September 2019, the FDA’s Allergenic Products Advisory Committee (APAC) voted to support Palforzia’s use in children and teens with peanut allergy. The FDA’s decision is expected in early 2020.
Rose Joachim
, PhD, a Senior Healthcare Analyst at GlobalData, told BioSpace, “The FDA advisory committee’s strong support for Aimmune’s Palforzia suggests that despite the drug not being a perfect fit for every patient with a peanut allergy, the therapy still has great potential to address key unmet needs in the US.”
Viaskin Peanut [DBV Technologies] – epicutaneous immunotherapy (EPIT)
Viaskin Peanut is a patch worn on the skin that delivers very small amounts of peanut allergen (usually microgram amounts versus milligram quantities used in oral immunotherapy) into the top few layers of skin, allowing the immune system to interact with the antigen (in this case peanut protein). Epicutaneous immunotherapy offers benefits over oral immunotherapy, such as using much lower doses of antigen, avoiding allergen ingestion, and having less systemic side effects.
Viaskin Peanut received Fast Track Designation in 2012 followed by Breakthrough Designation in 2015. However, DBV hit a mild bump in the road in October 2017 when their Phase 3 trial, Peanut Epicutaneous Immunotherapy (EPIT) Efficacy and Safety (PEPITES), failed to meet the primary endpoint - a “15 percent lower bound of the confidence interval” between response rates in the patch and placebo groups. Despite missing the preset mark, the Viaskin Peanut patch significantly improved desensitization: 35 percent of participants ages 4-11 who wore the Viaskin patch containing 250 μg peanut protein were desensitized at the food challenge at the end of the study versus 14 percent of participants who wore a placebo patch. Viaskin Peanut was also well-tolerated and the withdrawal percentage was low in each group: only 10.5 percent of the Viaskin-wearing participants and 9.3 percent of the placebo-wearing participants dropped out.
Another Phase 3 study, Real Life Use and Safety of Epicutaneous Immunotherapy (REALISE), studied the safety of Viaskin Peanut (250 μg) in 393 participants ages 4-11 in a routine clinical setting. The results agreed with other studies and showed that it was well-tolerated with serious adverse events occurring in only 3 participants (1 percent) who wore the Viaskin patch and 2 participants (2 percent) who wore the placebo patch. The most commonly reported side effect was mild to moderate local application site reactions.
DBV has various other ongoing trials, including the Phase 3 Epicutaneous Immunotherapy in Toddlers with Peanut Allergy (EPITOPE) study looking at the safety and efficacy of Viaskin Peanut (250 μg and 100 μg) in participants ages 1-3.
Despite the desensitization difference not being statistically significant between Viaskin Peanut and the placebo patch, DBV continued testing and still pursued FDA approval by filing a BLA in October 2018. It was poised to be the first peanut allergy drug to enter the market with an FDA decision expected in August 2019, but DBV Technologies withdrew its BLA in December 2018. This decision was made after consulting with the FDA, based on questions raised by the agency and the need for more manufacturing data, not due to any safety concerns. DBV submitted a new BLA in August 2019, which was accepted by the FDA in early October 2019. The FDA aims to review the BLA by August 5, 2020.
“Although Viaskin Peanut’s epicutaneous therapy has failed to demonstrate the same degree of efficacy in comparison to Palforzia, Viaskin Peanut’s safety profile may afford it a unique niche in the market,” Joachim added. “This includes the treatment of patients with extreme peanut sensitivity, who otherwise might not qualify for treatment with oral immunotherapy, as well as small children.”
Phase 2
CA002 [Camallergy] – oral immunotherapy (OIT)
CA002 is a peanut protein-based biological drug for oral immunotherapy, much like Palforzia. The initial dosing stage is set up slightly differently (a single dose at the initial appointment and a 7-stage dose escalation period completed in 4 months or less), but the overall idea of increasing the dose of peanut protein and then maintaining a steady dose indefinitely is the same.
Their proof-of-concept Phase 1 trial, Study of Tolerance to oral Peanut (STOP), studied the safety and efficacy of CA002 in 22 UK children ages 4-17 with peanut allergy. All 22 children gradually increased dosing every 2 weeks, then the 800 mg maintenance dose was maintained for 30 weeks. Eighty-six percent of participants (19 of 22) tolerated the dose increases and maintenance doses at 800 mg, while 9 percent (2 participants) tolerated dose increases and maintenance doses up to 400 mg. Only 1 participant (5 percent) withdrew from the study. Reactions occurred in 86 percent of participants with most being mild and none being serious adverse events. At the end of the 30-week maintenance period, 64 percent of participants (14 of 22) could tolerate 6,600 mg of peanut protein, which is a 1000-fold increase from the median initial tolerated amount (6 mg).
The Phase 2 STOP2 trial showed the safety and efficacy of CA002 compared to standard of care (peanut avoidance) in UK children ages 7-16. In the first phase of the study, 62 percent of participants (24 of 39) who received CA002 could tolerate 1400 mg of peanut protein compared to none of the 46 participants who received standard of care. Eighty-four percent of participants who received CA002 could tolerate an 800 mg daily dose of peanut protein. In the second phase, the standard of care participants received CA002. Fifty-four percent and 91 percent could tolerate 1400 mg and 800 mg, respectively, of peanut protein. Mild side effects occurred in most patients, with gastrointestinal symptoms being the most common (31 participants had nausea and 31 had vomiting).
The STOP3 Phase 3 trial is not yet enrolling but will look at the safety and efficacy of CA002 in participants ages 4 and older with peanut allergy.
“Although it has shown promise in early phase clinical studies, at this point it is unclear how CA002 will be able to differentiate from Palforzia, which is already so much further ahead in development,” Joachim commented.
PRT100 [ProTA Therapeutics] – oral immunotherapy (OIT) and probiotic combination
PRT100 is a unique combination of peanut protein oral immunotherapy and a probiotic (the bacteria Lactobacillus rhamnosus). This combination therapy specifically leverages the immune-altering actions of probiotic bacteria to shift a patient’s immune response away from peanut allergy towards tolerance and sustained unresponsiveness (remission) – essentially a cure.
“Aimmune’s Palforzia and DBV’s Viaskin Peanut might be the biggest names in the news, but other later-stage products could prove to be important additions to the market because they address some of the pioneering products’ weaker points, especially the requirement for ongoing maintenance therapy to ensure protective desensitization against peanuts,” Joachim said. “One of the most exciting products in this regard is PRT100.”
The effects of probiotics on allergies have been studied previously. Lactobacillus rhamnosus, specifically, has been shown to prevent pollen-induced asthma in mice and even reduce airway allergies in mice whose mothers were exposed to the bacteria while they were pregnant. These results make Lactobacillus rhamnosus an interesting agent for allergy treatment.
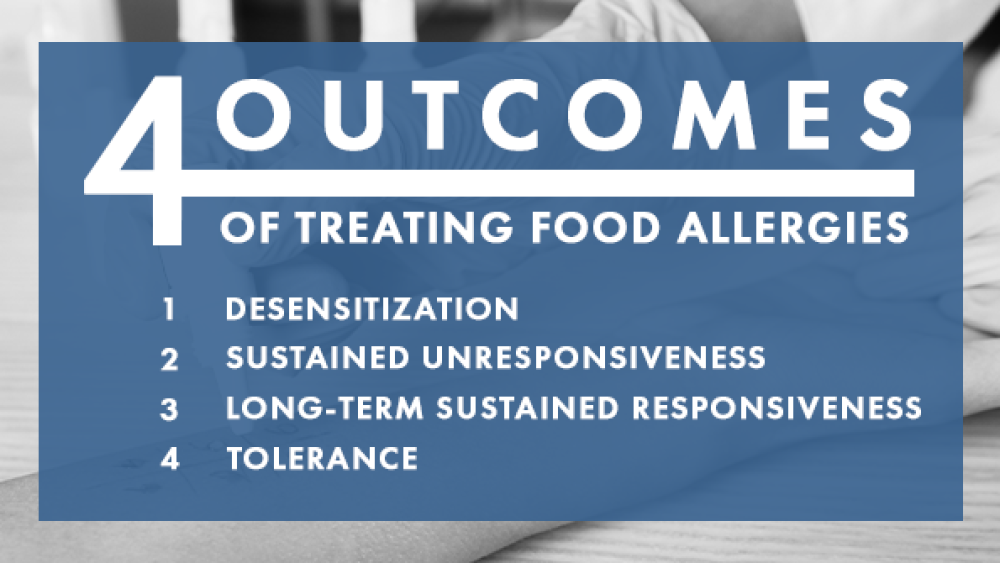
There are four possible outcomes to treating food allergies. Desensitization is the increased reaction threshold to an allergen, which requires continues therapy to maintain its effects. Sustained unresponsiveness, also called remission, is thought to be a “reprogramming of the immune response to the allergen” where one can tolerate the allergen weeks or months after treatment is stopped. Long-term sustained responsiveness is the ability to tolerate the antigen years after the treatment stopped and may suggest possible tolerance but non-responsiveness to allergen can’t be guaranteed. Finally, tolerance is the complete and “permanent” lack of response to an allergen after treatment is stopped (although “permanent” is usually a subjective amount of time).
The Phase 2a proof-of-concept trial in 62 Australian children ages 1-10 evaluated how many children showed sustained unresponsiveness (remission) up to 2-5 weeks after stopping PRT100 treatment. The participants either received PRT100 (31 children) or placebo (31 children) for 18 months following an 8-month dose escalation and 10-month maintenance phase oral immunotherapy schedule. Ninety percent of participants (26 of 29) who received PRT100 were desensitized to 4 g of protein powder on the last day of maintenance treatment compared to 7 percent of participants (2 of 28) who received a placebo. Those patients were examined 2-5 weeks after stopping treatment for sustained unresponsiveness, which was seen in 82 percent of participants (23 of 28) who received PRT100 compared to 3 percent of participants (1 of 28) who received a placebo. All but 1 patient who achieved sustained unresponsiveness was still consuming anywhere from 5 peanuts to 3 tablespoons per week without allergic reaction 3 months after treatment ended. Not surprisingly, more PRT100-treated participants reported adverse events than those taking a placebo (34 taking PRT100 and 15 taking placebo).
Forty-eight children from this proof-of-concept study were enrolled in a 4-year follow-up study to track their sustained unresponsiveness. Of the participants who achieved sustained unresponsiveness at the end of the proof-of-concept trial, 70 percent had long-lasting tolerance 4 years after stopping treatment. Many more participants who received PRT100 continued to eat peanuts (16 of 24 participants, 67 percent) compared to participants who received placebo (1 of 24 participants, 4 percent).
A Phase 2b trial in 200 Australian children ages 1-10 is evaluating the sustained unresponsiveness (remission) rate in a larger population. This trial is not only comparing PRT100 to a placebo but also to regular peanut oral immunotherapy (without probiotics). All 200 participants were enrolled as of May 2018 and the study is currently ongoing.
“With top-line results from this trial expected in Q1 2020, the field will soon learn whether PRT100’s success in early phase trials can be replicated in a larger population of patients,” Joachim added. “If successful, it could have enormous implications for the field.”
Dupixent (Dupilumab) [Regeneron] – anti-IL-4R antibody
Dupixent is an injectable anti-interleukin-4 receptor (IL-4R) antibody currently approved for atopic dermatitis, asthma, and chronic rhinosinusitis with nasal polyposis (CRSwNP). IL-4R is a protein involved in immune response, specifically IL-4 and IL-13 signaling, which regulates IgE production and, ultimately, allergic responses. Dupixent is also being developed for peanut and grass pollen allergy (among other indications) in collaboration with Sanofi.
A currently recruiting Phase 2 trial is studying whether Dupixent can increase peanut protein tolerability compared to placebo in an estimated 48 children ages 6-17.
Interestingly, Regeneron, Sanofi, and Aimmune announced a partnership in October 2017 to study Dupixent with Palforzia as a combination therapy. A currently recruiting Phase 2 trial is expected to enroll 156 children 6-17 years old to study whether Palforzia with Dupixent improves desensitization to 2044 mg of peanut protein compared to Palforzia with placebo. Whether the Dupixent-Palforzia combination induces sustained unresponsiveness will also be explored.
“Several monoclonal antibodies are in development for peanut allergy, including Sanofi/Regeneron’s Dupixent,” Joachim said. “Although these types of agents could be useful tools in limiting the side effects of peanut immunotherapy, it is unclear how practical the use of expensive biologics will be in the long-term treatment of peanut allergy.”
Etokimab (ANB020) [AnaptysBio] – anti-IL-33 antibody - no longer being pursued for peanut allergy
Etokimab, previously called ANB020, is also not specific to peanut allergy – it is an anti-interleukin 33 (IL-33) antibody. IL-33 is an immune system protein (called a proinflammatory cytokine) that plays a role in many allergic diseases, such as atopic dermatitis, food allergies, and asthma. Etokimab was previously shown to be well-tolerated and safe in 96 healthy volunteers administered either subcutaneously or intravenously.
A proof-of-concept Phase 2a study in 20 participants with moderate to severe peanut allergy showed debatably positive results. Forty-seven percent of participants (7 of 15) who received one dose of Etokimab could tolerate 500 mg of peanut protein 14 days after administration compared to 40 percent of participants (2 of 5) who received a placebo. After removing four patients, two patients from each group, because they “exhibited mild symptoms at baseline,” the data looked much more impressive: 46 percent of participants (6 of 13 who received Etokimab could tolerate 500 mg of peanut protein compared to none of the 3 participants who received a placebo.
Although AnaptysBio was reported to be planning a Phase 2b study, the company decided against pursuing Etokimab for peanut allergy in mid-2018. Peanut allergy is also not listed as an indication for Etokimab on the company’s website. However, Markets Insider said AnaptysBio “may pursue potential investigator-sponsored trials of Etokimab” for peanut allergy.
Early-stage drug highlights
As for drugs in earlier-stage development, there are a few innovative options, including Introimmune Therapeutics’ peanut-containing toothpaste as oral mucosal immunotherapy and Vendanta Biosciences’ human microbiota-derived bacteria drug VE416. A Phase 1b/2 trial studying VE416 alone and in combination with peanut oral immunotherapy is currently ongoing and is expected to enroll 40 participants ages 12-55. The trial began enrolling in July 2019.
“There are a number of products in early clinical development with the potential to shape the peanut allergy market going forward,” Joachim said. “This includes a variety of injectable allergen immunotherapy products, which look more similar to the allergy shots patients typically receive for seasonal allergies. While original attempts at injectable immunotherapy for peanut allergy led to dangerous side effects, the current products in development seek to avoid and abate the allergic response.”
Aravax’s PVX108, an intradermal immunotherapy vaccine for peanut allergy, is one such drug. It contains peptides that mimic portions of major peanut allergens that can train the immune system specifically, which largely reduces the risk of allergic side effects. The company announced that a Phase 1 trial showed that PVX108 was safe and well-tolerated.
Outlook
With the high unmet need in the peanut allergy field and multiple late-stage drugs knocking on the FDA’s door for approval, it may not be surprising that the market for peanut allergy drugs seems very bright. GlobalData is forecasting the peanut allergy market to grow an astounding 1,700-fold from 2017-2027 – expanding from a $2.6 million industry in 2017 to a $4.5 billion industry by 2027.
However, the price tag of these drugs must be considered, as they will likely be a lifelong drug. The Institute for Clinical and Economic Review (ICER) published a report in April 2019 discussing the potential pricing of AR101 and Viaskin Peanut. The ICER estimated AR101 would cost $8,700 for the first year and $4,200 for each year of maintenance, in comparison to Viaskin Peanut’s estimated cost of $6,500 per year.
Oral immunotherapy is not a new idea – about 200 of the 5,000 board-certified allergists in the US already use oral immunotherapy to treat food allergies, including peanut allergy, by using products sold from retail stores, such as peanut flour. Although buying a bag of peanut flour from the grocery store is much cheaper, some allergists emphasize the importance of a standard product and protocol that should give more predictable results and be safer for patients.
Despite celebration about the potential new therapies coming to market, some families and doctors are debating how useful these drugs, especially oral immunotherapy-based ones, will be for patients. It is important to remember that these drugs do not offer a cure, they have side effects, and may not work for everyone. However, they may provide more protection against severe allergic reactions from accidental peanut exposure and, therefore, some peace of mind for patients.