MEMPHIS, Tenn., Nov. 18, 2015 /PRNewswire/ -- The most detailed analysis yet of the role germline mutations in genes associated with cancer predisposition play in the development of childhood cancer suggests that comprehensive genomic screening may be warranted on all pediatric cancer patients, not just those with a family history of cancer. The study from the St. Jude Children's Research Hospital Washington University Pediatric Cancer Genome Project appears in the November 19 edition of the New England Journal of Medicine.
Experience the interactive Multimedia News Release here: http://www.multivu.com/players/English/7692851-st-jude-hospital-genome-project/
Ultimately, researchers anticipate that systematic monitoring of patients and family members who have germline mutations in cancer predisposition genes will allow the detection of cancers at their earliest and most curable stage, thereby improving the outcomes for these children and family members.
Researchers conducted next-generation DNA sequencing of both the tumor and normal tissues from 1,120 pediatric cancer patients and found that 8.5 percent of patients had pathogenic or likely pathogenic mutations of genes within their normal tissue that increase their risk of developing cancer. Prior to this study, the presence of such germline mutations in pediatric cancer patients was thought to be extremely rare and restricted to children in families with strong histories of cancer. This study revealed that more than half of the children with germline mutations lacked any family history of cancer.
"This paper marks an important turning point in our understanding of pediatric cancer risk and will likely change how patients are evaluated," said corresponding author James R. Downing, M.D., St. Jude president and chief executive officer. "For many pediatric cancer patients, comprehensive next-generation DNA sequencing of both their tumor and normal tissue may provide valuable information that will not only influence their clinical management but also lead to genetic counseling and testing of their parents and siblings who may be at risk and would benefit from ongoing surveillance.
"The frequency of 8.5 percent represents our current estimate of the number of pediatric patients with a hereditary cancer predisposition," Downing added. "This number will likely increase as we learn more about mutations in this class of genes in young cancer patients." To accomplish the latter, St. Jude has initiated a new clinical research study, Genomes for Kids (G4K), which incorporates an unparalleled level of next-generation sequencing into the medical workup of every eligible pediatric cancer patient who enters the hospital for treatment.
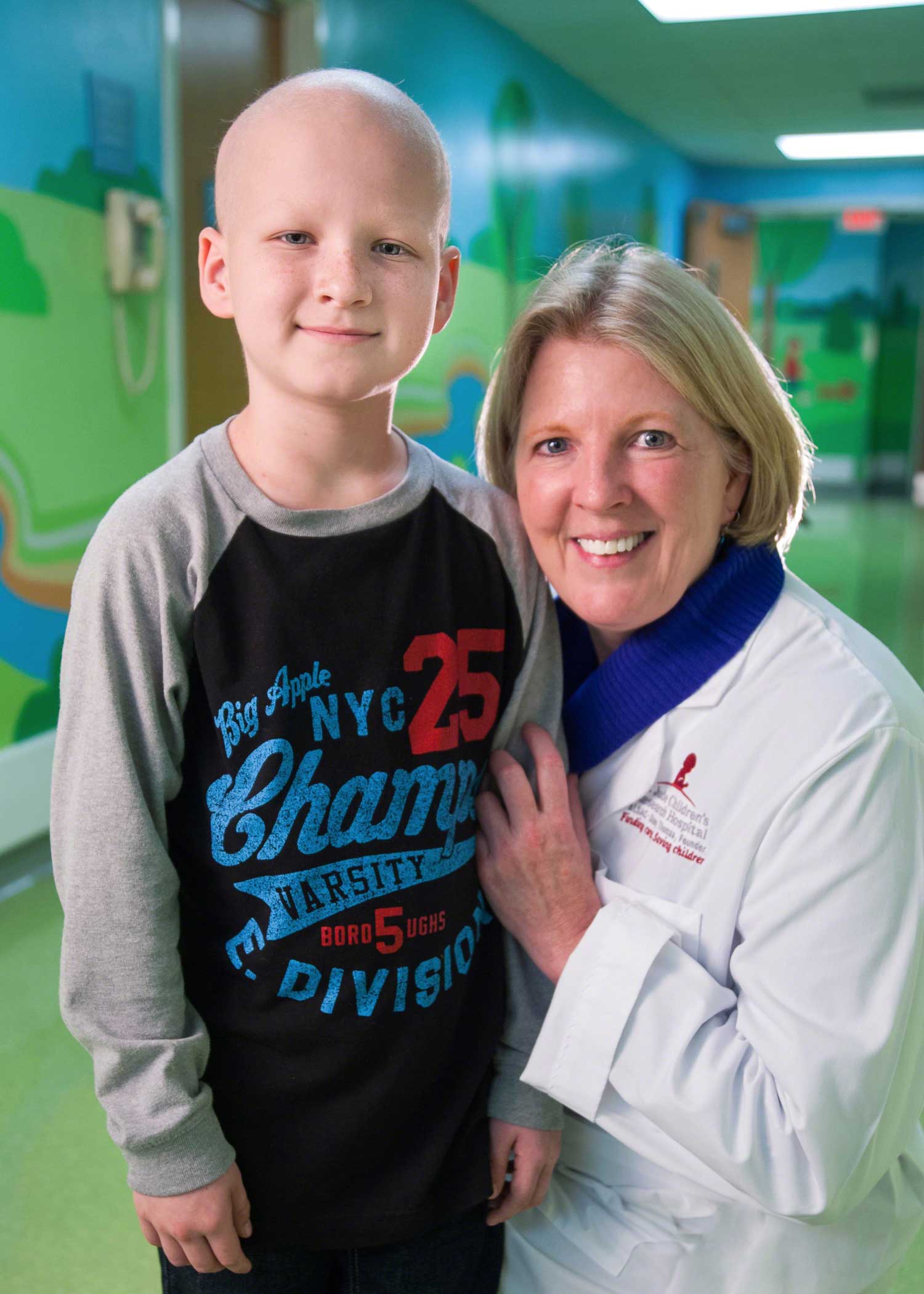
Any child found to have a germline mutation in a cancer predisposition gene will be referred to the new St. Jude Hereditary Cancer Predisposition Clinic, which evaluates and cares for children who are at increased genetic risk for cancer. The clinic is staffed by a team of doctors, nurses and genetic counselors who work with families to determine if a child's cancer might be inherited. The staff then collaborates with other St. Jude doctors and researchers to find new and better ways to help families with an elevated cancer risk. This new clinic is one of only a few programs in the world focused on evaluating and managing children and families with known or suspected cancer predisposition.
"Our study inthe New England Journal of Medicine lays the groundwork to understand the spectrum of cancers and age-specific cancer risks associated with germline mutations in predisposition genes and how best to monitor at-risk patients and families," said co-author Kim Nichols, M.D., a member of the St. Jude Department of Oncology and director of the St. Jude Hereditary Cancer Predisposition Clinic.
Co-author Richard K. Wilson, Ph.D., director of the McDonnell Genome Institute at Washington University School of Medicine in St. Louis, added: "We've suspected for some time that many pediatric cancers could be traced to an inherited genetic predisposition. Now, using genome sequencing, we can see the contribution of germline mutations to pediatric cancer risk. Our results explain why children, who have not lived long enough to accumulate a critical number of cancer-causing mutations can still develop cancer."
About the Study and Genetic Sequencing
The human genome is encoded in the DNA that carries the instructions required to assemble and sustain life. Whole-genome sequencing involves determining the exact order of the 3 billion nucleotides that make up human DNA. Whole-exome sequencing involves sequencing the 1 to 2 percent of the human genome that carries the approximately 20,000 human genes.
This study involved sequencing the whole genome, whole exome or both of patients enrolled in the Pediatric Cancer Genome Project to check for germline mutations in 565 genes associated with cancer. In-depth data analysis was done on 60 of these genes that are associated with autosomal dominant hereditary cancer predisposition syndromes. Mutations in these genes are known to increase cancer risk when one of the two copies of the gene is altered.
In this study, 95 patients, or 8.5 percent, had germline mutations in 21 of the 60 genes. Investigators checked whole-exome sequencing data of a comparison group without cancer and found that only 1.1 percent of 966 adults enrolled in the 1000 Genomes Project, an international collaboration to map human genetic variation, had alterations in the same genes.
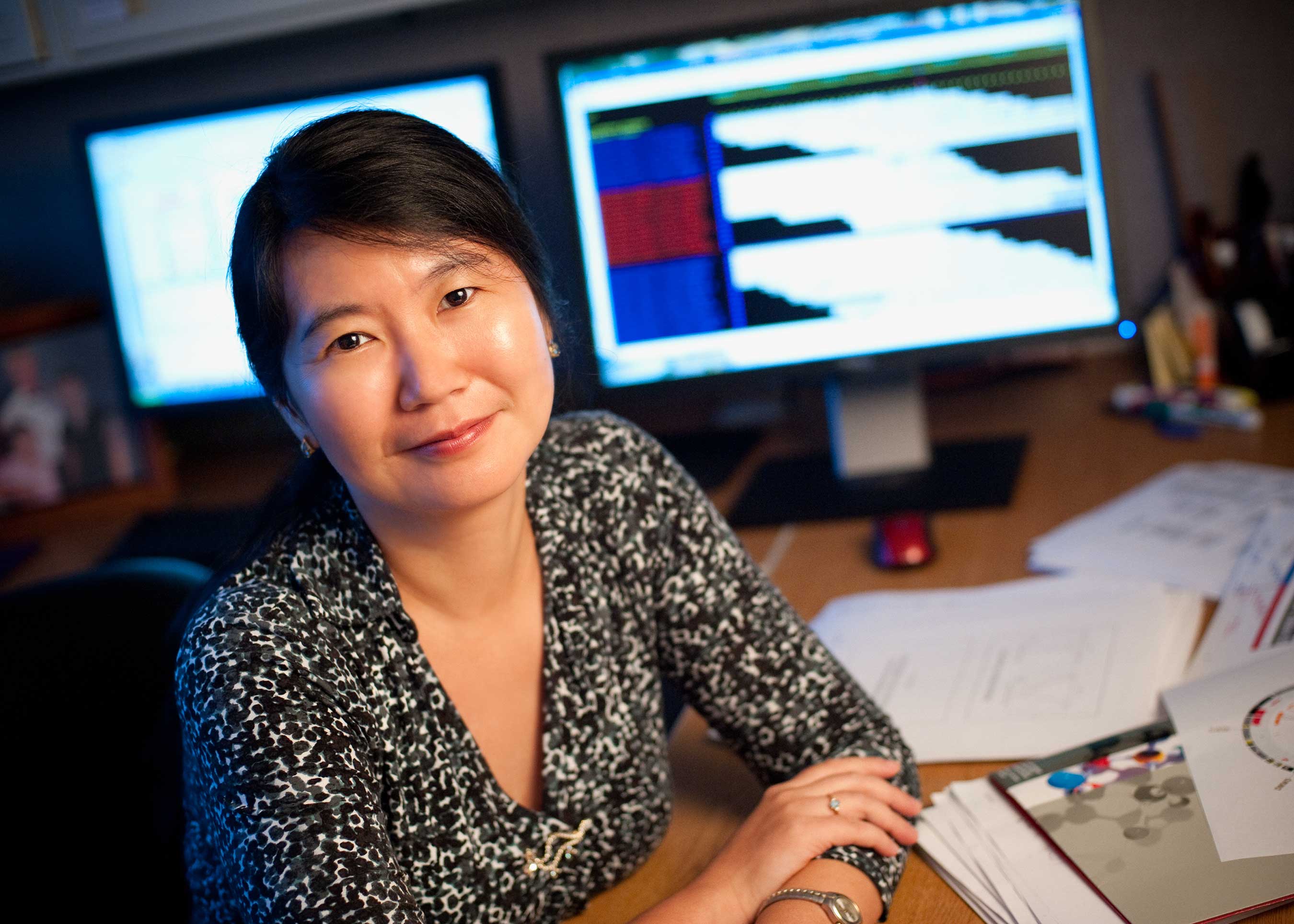
The genes selected for detailed analysis were chosen based on a review of available cancer and genetic databases, the medical literature and other information. "Finding genomic variants is relatively easy compared to assessing their cancer-causing potential," said co-first author Jinghui Zhang, Ph.D., chair of the St. Jude Department of Computational Biology. "The system we developed to create the database for this study provides a template for assessing the pathogenic significance of alterations going forward."
In this study, the frequency of germline mutations in cancer predisposition genes varied by the type of cancer the child had. The highest frequency, 16.7 percent, was found in children with non-central nervous system (CNS) solid tumors, followed by CNS tumors, 9 percent, and leukemia, 4.4 percent.
The most commonly mutated genes in the affected patients were TP53, APC, BRCA2, NF1, PMS2 and RB1. Many of these genes have been previously associated with rare families with multiple children who develop cancer. An unexpected finding was the identification of mutations in the breast and ovarian cancer genes BRCA1 and BRCA2 in a number of the pediatric cancer patients. These genes are not currently included in pediatric cancer genetic screening. The prevalence of mutations in these genes in this pediatric cancer cohort suggests that the role of these genes in pediatric cancer needs to be further studied. "Another surprising finding to emerge from this study was the prevalence of germline mutations in six patients with Ewing sarcoma, a cancer of the bone and soft tissue that was not previously thought to be part of any cancer predisposition syndrome," Nichols said.
The other co-first authors are Gang Wu, Ph.D., of St. Jude, and Michael Walsh, M.D., formerly of St. Jude and now of Memorial Sloan Kettering Cancer Center, New York. The other authors are Michael Edmonson, Tanja Gruber, John Easton, Dale Hedges, Xiaotu Ma, Xin Zhou, Donald Yergeau, Mark Wilkinson, Bhavin Vadodaria, Xiang Chen, Rose McGee, Stacy Hines-Dowell, Regina Nuccio, Emily Quinn, Sheila Shurtleff, Michael Rusch, Aman Patel, Jared Becksfort, Shuoguo Wang, Amar Gajjar, David Ellison, Alberto Pappo and Ching-Hon Pui, all of St. Jude; Meaghann Weaver, formerly of St. Jude; and Li Ding and Elaine Mardis, both of the McDonnell Genome Institute, Washington University, St. Louis.
The research was funded in part by the Pediatric Cancer Genome Project, including Kay Jewelers, a lead sponsor; a grant (CA021765) from the National Cancer Institute at the National Institutes of Health; and ALSAC.
St. Jude Children's Research Hospital
St. Jude Children's Research Hospital is leading the way the world understands, treats and cures childhood cancer and other life-threatening diseases. It is the only National Cancer Institute-designated Comprehensive Cancer Center devoted solely to children. Treatments developed at St. Jude have helped push the overall childhood cancer survival rate from 20 percent to 80 percent since the hospital opened more than 50 years ago. St. Jude freely shares the breakthroughs it makes, and every child saved at St. Jude means doctors and scientists worldwide can use that knowledge to save thousands more children. Families never receive a bill from St. Jude for treatment, travel, housing and foodbecause all a family should worry about is helping their child live. To learn more, visit stjude.org or follow St. Jude at @stjuderesearch.
Washington University
Washington University School of Medicine's 2,100 employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient-care institutions in the nation, currently ranked sixth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children's hospitals, the School of Medicine is linked to BJC HealthCare.

To view the original version on PR Newswire, visit:http://www.prnewswire.com/news-releases/new-study-suggests-more-than-8-percent-of-children-with-cancer-have-genetic-predisposition-300181427.html
SOURCE St. Jude Children's Research Hospital

