Three Late Breaking Science Presentations from MAPLE-HCM Provide Additional Data Including Responder Analyses, Patient Reported Outcomes, and Cardiac Biomarkers
SOUTH SAN FRANCISCO, Calif., Nov. 10, 2025 (GLOBE NEWSWIRE) -- Cytokinetics, Incorporated (Nasdaq: CYTK) today announced that additional data from MAPLE-HCM (Metoprolol vs Aficamten in Patients with LVOT Obstruction on Exercise Capacity in HCM) were presented in three Late Breaking Science sessions at the Hypertrophic Cardiomyopathy Medical Society Scientific Sessions and the American Heart Association Scientific Sessions 2025 in New Orleans, LA. Two of the presentations were simultaneously published in the Journal of the American College of Cardiology.1,2
“These additional analyses from MAPLE-HCM expand on the primary finding that aficamten is superior to metoprolol on exercise capacity, with new insights into the overall treatment effect of aficamten as well as its effect on symptoms and biomarkers in comparison to metoprolol,” said Fady I. Malik, M.D., Ph.D., Cytokinetics’ Executive Vice President of Research & Development. “What’s notable is patients treated with aficamten achieved a significantly greater number of clinical response categories compared with metoprolol, and that nearly 40% achieved significant improvements in patient reported symptoms.”
Responder Analysis Shows Significantly More Patients on Aficamten Achieved Positive or Complete Response Compared to Metoprolol
Andrew Wang, M.D., Cardiologist and Professor of Medicine, Duke University School of Medicine presented a pre-specified responder analysis from MAPLE-HCM evaluating five clinically relevant measures of disease burden: complete hemodynamic response, symptom improvement, cardiac biomarker response, enhanced exercise capacity and favorable cardiac remodeling. These results were also simultaneously published in the Journal of the American College of Cardiology.1
After 24 weeks of treatment, aficamten was associated with greater improvements than metoprolol in all outcome measures (all p<0.001) (Figure 1). Additionally, the proportion of patients who had a positive response (improvement in three or four clinical parameters) or a complete response (improvement in all five clinical parameters) was 78% in those receiving aficamten vs. 3% for those receiving metoprolol (p<0.001).
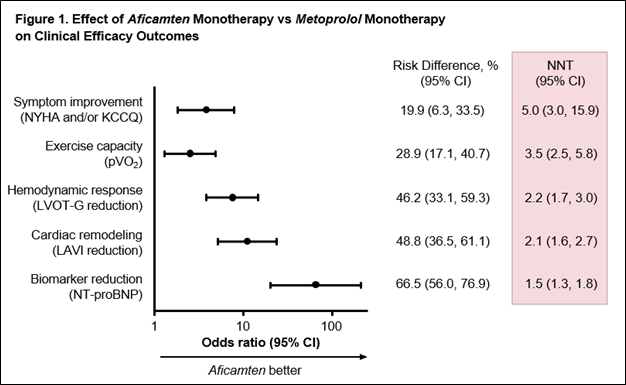
KCCQ, Kansas City Cardiomyopathy Questionnaire; LAVI, left atrial volume index; LVOT-G, left ventricular outflow tract gradient; NNT, number needed to treat; NT-proBNP, N-terminal pro–B-type natriuretic peptide; NYHA, New York Heart Association
As previously disclosed, in MAPLE-HCM the rate of adverse events (AEs) was similar between groups. At least one treatment-emergent AE was reported by 65 (73.9%) and 66 (75.9%) patients treated with aficamten and metoprolol, respectively. The most common AE reported in the aficamten group in excess of the comparator (>5%) was hypertension (9 [10.2%] patients on aficamten compared to 2 [2.3%] patients on metoprolol) and the most common AE reported in the metoprolol group in excess of the comparator was dizziness (15 [17.2%] patients on metoprolol compared to 5 [5.7%] patients on aficamten).
Analysis of Patient Reported Outcomes Expands on Effect of Aficamten on Patient Symptom Burden
Michael E. Nassif, M.D., Cardiologist, Saint Luke’s Mid America Heart Institute, Associate Professor of Medicine, University of Missouri Kansas City presented results from a pre-specified sub-study of two patient reported outcome instruments in MAPLE-HCM: the Kansas City Cardiomyopathy Questionnaire (KCCQ) and Seattle Angina Questionnaire Summary Score (SAQ). The results from this analysis were also simultaneously published in the Journal of the American College of Cardiology.2
At 24 weeks, treatment with aficamten resulted in significantly greater improvements than metoprolol in both KCCQ Overall Summary Score (KCCQ-OSS) (16.6 points vs. 8.9 points, respectively; between-group difference = 7.8 points [95% CI: 3.3 to 12.3; p=0.001]) and KCCQ Clinical Summary Score (KCCQ-CSS) (15.8 points vs. 8.7 points, respectively; between-group difference = 6.9 points [95% CI: 2.6 to 11.2; p=0.002]).
Aficamten was also associated with statistically significant improvements across all KCCQ domains (p<0.05). Patients on aficamten more frequently reported very large improvements in KCCQ-OSS, defined as ≥20-point improvement (38.6% vs. 18.4%; number needed to treat (NNT)=4.9), and were significantly less likely to experience a worsening in KCCQ-OSS than those treated with metoprolol (6.8% vs 18.4%; number needed to harm (NNH)=8.6).
A non-statistically significant trend for greater improvement in SAQ-SS was observed with aficamten (13.9 vs. 8.4 [adjusted between-group difference = 4.6 points; 95% CI: -0.3 to 9.5; p=0.063]), driven by a large and statistically significant improvement in the SAQ Physical Limitation Domain, where patients on aficamten improved by a mean of 18.7 points compared with 6.9 points for those on metoprolol (between-group difference = 10.1 points; 95% CI: 3.9 to 16.2; p=0.001). Changes in the SAQ Angina Frequency and Quality of Life Domains were similar between treatment groups.
Aficamten Associated with Statistically Significant Improvement in Cardiac Biomarkers Compared to Metoprolol
Neal K. Lakdawala, M.D., Cardiovascular Medicine, Brigham and Women’s Hospital, Harvard Medical School presented a pre-specified supplemental analysis from MAPLE-HCM of the impact of treatment with aficamten compared to metoprolol on the cardiac biomarkers NT-proBNP and high sensitivity cardiac troponin I (hs-cTnI). At baseline, high NT-proBNP and high hs-cTnI, indicative of cardiac wall stress and myocardial injury, respectively, were strongly correlated and generally associated with worse diastolic dysfunction. After treatment for 24 weeks, aficamten was associated with a 73% reduction (p<0.001) from baseline in NT-proBNP compared to an increase of 42% observed in patients receiving metoprolol (-81% treatment effect, p<0.001). Similarly, aficamten was associated with a 43% reduction in hs-cTnI, compared to a 17% decrease for metoprolol (-28% treatment effect, p=0.001). Patients with the greatest reductions in NT-proBNP experienced greater improvements in peak oxygen uptake (pVO2) and ventilatory efficiency (VE/VCO2). Additionally, changes in NT-proBNP were correlated with reductions of left ventricular outflow tract gradients (LVOT-G) and improved health status (KCCQ-OSS).
About Aficamten
Aficamten is an investigational selective, small molecule cardiac myosin inhibitor discovered following an extensive chemical optimization program that was conducted with careful attention to therapeutic index and pharmacokinetic properties.3 Aficamten was designed to reduce the number of active actin-myosin cross bridges during each cardiac cycle and consequently suppress the myocardial hypercontractility that is associated with HCM. In preclinical models, aficamten reduced myocardial contractility by binding directly to cardiac myosin at a distinct and selective allosteric binding site, thereby preventing myosin from entering a force producing state.
The development program for aficamten is assessing its potential as a treatment that improves exercise capacity as measured by peak oxygen uptake (pVO2) and relieves symptoms in patients with HCM. Aficamten was evaluated in SEQUOIA-HCM, a positive pivotal Phase 3 clinical trial in patients with symptomatic obstructive hypertrophic cardiomyopathy (HCM). Aficamten received Breakthrough Therapy Designation for the treatment of symptomatic HCM from the U.S. Food & Drug Administration (FDA) and for the treatment of symptomatic obstructive HCM from the National Medical Products Administration (NMPA) in China.
Aficamten is also currently being evaluated in ACACIA-HCM, a Phase 3 clinical trial of aficamten in patients with non-obstructive HCM; CEDAR-HCM, a clinical trial of aficamten in a pediatric population with oHCM; and FOREST-HCM, an open-label extension clinical study of aficamten in patients with HCM.
Disclaimer
This communication contains a summary of new data related to the clinical development of aficamten presented at the Hypertrophic Cardiomyopathy Medical Society Scientific Sessions and the American Heart Association Scientific Sessions 2025. Aficamten is an investigational drug and is not approved by any regulatory agency. Its safety and efficacy have not been established. Aficamten is currently under regulatory review in the U.S, where the FDA is reviewing a New Drug Application (NDA) for aficamten with a Prescription Drug User Fee Act (PDUFA) target action date of December 26, 2025. Additionally, the European Medicines Agency (EMA) is reviewing a Marketing Authorization Application (MAA) for aficamten, and The Center for Drug Evaluation (CDE) of the China National Medical Products Administration (NMPA) is reviewing an NDA for aficamten with Priority Review.
About Hypertrophic Cardiomyopathy
Hypertrophic cardiomyopathy (HCM) is a disease in which the heart muscle (myocardium) becomes abnormally thick (hypertrophied). The thickening of cardiac muscle leads to the inside of the left ventricle becoming smaller and stiffer, and thus the ventricle becomes less able to relax and fill with blood. This ultimately limits the heart’s pumping function, resulting in reduced exercise capacity and symptoms including chest pain, dizziness, shortness of breath, or fainting during physical activity. HCM is the most common monogenic inherited cardiovascular disorder, with approximately 280,000 patients diagnosed, however, there are an estimated 400,000-800,000 additional patients who remain undiagnosed in the U.S.4,5,6 Two-thirds of patients with HCM have obstructive HCM (oHCM), where the thickening of the cardiac muscle leads to left ventricular outflow tract (LVOT) obstruction, while one-third have non-obstructive HCM (nHCM), where blood flow isn’t impacted, but the heart muscle is still thickened. People with HCM are at high risk of also developing cardiovascular complications including atrial fibrillation, stroke and mitral valve disease.7 People with HCM are at risk for potentially fatal ventricular arrhythmias and it is one of the leading causes of sudden cardiac death in younger people or athletes.8 A subset of patients with HCM are at high risk of progressive disease leading to dilated cardiomyopathy and heart failure necessitating cardiac transplantation.
About Cytokinetics
Cytokinetics is a specialty cardiovascular biopharmaceutical company, building on its over 25 years of pioneering scientific innovations in muscle biology, and advancing a pipeline of potential new medicines for patients suffering from diseases of cardiac muscle dysfunction. Cytokinetics is readying for potential regulatory approvals and commercialization of aficamten, a cardiac myosin inhibitor, following positive results from SEQUOIA-HCM, the pivotal Phase 3 clinical trial in patients with obstructive hypertrophic cardiomyopathy (HCM). Aficamten is also being evaluated in additional clinical trials enrolling patients with obstructive and non-obstructive HCM. In addition, Cytokinetics is developing omecamtiv mecarbil, a cardiac myosin activator, in patients with heart failure with severely reduced ejection fraction (HFrEF), ulacamten, a cardiac myosin inhibitor with a mechanism of action distinct from aficamten, for the potential treatment of heart failure with preserved ejection fraction (HFpEF) and CK-089, a fast skeletal muscle troponin activator with potential therapeutic application to a specific type of muscular dystrophy and other conditions of impaired skeletal muscle function.
For additional information about Cytokinetics, visit www.cytokinetics.com and follow us on X, LinkedIn, Facebook and YouTube.
Forward-Looking Statements
This press release contains forward-looking statements for purposes of the Private Securities Litigation Reform Act of 1995 (the "Act"). Cytokinetics disclaims any intent or obligation to update these forward-looking statements and claims the protection of the Act's Safe Harbor for forward-looking statements. Examples of such statements include, but are not limited to, statements relating to any of our clinical trials, statements relating to the potential benefits of aficamten or any of our other drug candidates, or our ability to obtain regulatory approval for aficamten in any jurisdiction by any particular date, if ever. Cytokinetics' research and development activities; the design, timing, results, significance and utility of preclinical and clinical results; and the properties and potential benefits of Cytokinetics' other drug candidates. Such statements are based on management's current expectations, but actual results may differ materially due to various risks and uncertainties, including, but not limited to, potential difficulties or delays in the development, testing, regulatory approvals for trial commencement, progression or product sale or manufacturing, or production of Cytokinetics' drug candidates that could slow or prevent clinical development or product approval; Cytokinetics' drug candidates may have adverse side effects or inadequate therapeutic efficacy; the FDA or foreign regulatory agencies may delay or limit Cytokinetics' ability to conduct clinical trials; Cytokinetics may be unable to obtain or maintain patent or trade secret protection for its intellectual property; standards of care may change, rendering Cytokinetics' drug candidates obsolete; and competitive products or alternative therapies may be developed by others for the treatment of indications Cytokinetics' drug candidates and potential drug candidates may target. For further information regarding these and other risks related to Cytokinetics' business, investors should consult Cytokinetics' filings with the Securities and Exchange Commission.
CYTOKINETICS® and the CYTOKINETICS and C-shaped logo are registered trademarks of Cytokinetics in the U.S. and certain other countries.
Contact:
Cytokinetics
Diane Weiser
Senior Vice President, Corporate Affairs
(415) 290-7757
References:
- Wang, A, Garcia-Pavia, P, Masri, A. et al. Aficamten in Obstructive Hypertrophic Cardiomyopathy: A Multi-Domain, Patient-Level Analysis of the MAPLE-HCM Trial. JACC. 2025.
- Nassif, M, Garcia-Pavia, P, Masri, A. et al. Effect of Aficamten vs Metoprolol on Patient-Reported Health Status in Obstructive Hypertrophic Cardiomyopathy. JACC. 2025
- Masri A, et al. Safety and Efficacy of Aficamten in Patients with Nonobstructive Hypertrophic Cardiomyopathy: A 96-Week Analysis from FOREST-HCM. J Card Fail. 2025
- Chuang C, Collibee S, Ashcraft L, et al. Discovery of Aficamten (CK-274), a Next-Generation Cardiac Myosin Inhibitor for the Treatment of Hypertrophic Cardiomyopathy. J Med Chem. 2021;64(19):14142–14152. https://doi.org/10.1021/acs.jmedchem.1c01290
- CVrg: Heart Failure 2020-2029, p 44; Maron et al. 2013 DOI: 10.1016/S0140-6736(12)60397-3; Maron et al 2018 10.1056/NEJMra1710575
- Symphony Health 2016-2021 Patient Claims Data DoF;
- Maron MS, Hellawell JL, Lucove JC, Farzaneh-Far R, Olivotto I. Occurrence of Clinically Diagnosed Hypertrophic Cardiomyopathy in the United States. Am J Cardiol. 2016; 15;117(10):1651-1654.
- Gersh, B.J., Maron, B.J., Bonow, R.O., Dearani, J.A., Fifer, M.A., Link, M.S., et al. 2011 ACCF/AHA guidelines for the diagnosis and treatment of hypertrophic cardiomyopathy. A report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Journal of the American College of Cardiology and Circulation, 58, e212-260.
- Hong Y, Su WW, Li X. Risk factors of sudden cardiac death in hypertrophic cardiomyopathy. Current Opinion in Cardiology. 2022 Jan 1;37(1):15-21
A photo accompanying this announcement is available at https://www.globenewswire.com/NewsRoom/AttachmentNg/8de3104b-50ad-4620-849f-73bfa6212075





