While Bruton’s tyrosine kinase inhibitors are often hailed as the next big breakthrough in multiple sclerosis, Immunic Therapeutics and others are leveraging neuroprotective targets and remyelination to keep the disease at bay.
One of the largest gatherings of multiple sclerosis researchers took place in Barcelona last month, as the space prepares to welcome a new class of treatment many believe will be a game-changer for patients.
Bruton’s tyrosine kinase (BTK) inhibitors are expected by many in the pharmaceutical industry to be the next big breakthrough in MS, Andreas Muehler, co-founder and chief medical officer at Immunic Therapeutics, told BioSpace. A number of BTK inhibitors—oral small molecule drugs that block B cell signaling to reduce inflammation in both the central nervous and the peripheral immune systems—are currently moving through Phase III trials, most notably Sanofi’s tolebrutinib, which has an FDA target action date of Dec. 28. If approved, tolebrutinib will become the first BTK inhibitor for MS.
Meanwhile, Roche is developing its own BTK inhibitor, fenebrutinib. The Swiss pharma presented data from the Phase II FENopta open-label extension trial at the 41st Congress of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS) last month, showing “near-complete” suppression of disease activity in patients with relapsing MS at 96 weeks. These results were largely consistent with one-year data from the same trial presented last September. Roche currently has three Phase III trials underway in relapsing MS and primary-progressive MS.
BTK inhibitors’ ability to cross the blood-brain barrier and penetrate the central nervous system (CNS) to slow neurodegeneration differentiates these treatments from biologics, which represent the top-selling drugs on the market. The ability to deliver these treatments orally could also allow for increased flexibility of dosing schedules compared to some current treatments that require injections.
Anti-Inflammatory and Beyond
Despite the high hopes for BTK inhibitors, safety concerns have created an environment of uncertainty around the class, according to industry watchers. Tolebrutinib and fenebrutinib have both been subject to partial clinical holds in the past three years due to cases of liver injury or indicated liver injury.
This leaves the door open for other approaches, including one being pursued by Immunic. The New York and Germany–based biotech is progressing vidofludimus calcium, which activates the Nurr1 protein, through Phase III trials.
When Immunic reported Phase II data from the asset in April, the biotech approached several companies about possible partnerships, “But this small industry group had decided that there is one mechanism of action, called BTK inhibitors, and that is the next big thing in MS,” Muehler said. “They believed that this type of drug would basically take care of all therapeutic needs in the space. We didn’t agree with that.”
According to Muehler, the most common current approach to treating MS is to pursue anti-inflammatory actions because inflammation in the brain leads to lesions. Brain lesions are the hallmark of active disease and are used to diagnose and monitor MS.
When Immunic began developing its lead candidate, this anti-inflammatory effect was the expected action of the drug. But when the biotech dug into its Phase II results, it saw the drug was having an effect beyond targeting inflammation, Muehler said. Further research revealed that vidofludimus calcium activated the Nurr1 protein—a mechanism associated with maintaining neuron health. Neurodegeneration occurs when levels of Nurr1 drop, he said.
Since pregnancy tends to be protective against MS, Immunic consulted a study to understand which genes were up- or down-regulated by this state. The research identified four genes of interest, including NR4A2, which encodes Nurr1and found NR4A2 to be strongly activated, Muehler said.
For Immunic, this meant the biotech had developed both an anti-inflammatory and a Nurr1 activator, which differentiates the drug from the other treatments that work solely through an anti-inflammatory effect.
This is why Immunic is testing the candidate in patients with progressive MS, as this group generally responds poorly to anti-inflammatory therapies. This type of study may demonstrate that Nurr1 activation is neuroprotective, Muehler said.
Results of this Phase II trial, announced in April, showed vidofludimus calcium reduced the relative risk of confirmed disability worsening events by 20% compared to placebo, with a 30% reduction in those patients with primary progressive MS.
In an oral presentation at ECTRIMS last month, Immunic shared further data from the Phase II trial showing that vidofludimus calcium significantly increased the likelihood of 24-week confirmed disability improvement overall, with benefits observed in both primary progressive MS and non-active secondary progressive MS subgroups.
If confirmed in Phase III studies, Muehler said a reduction in risk of worsening disability would be a landmark event for patients with progressive MS.
On the Brink
However, the long-term goal for MS research is to reverse disease progression or even discover a functional cure, Iain Greig, a reader in Medicinal Chemistry at the University of Aberdeen, told BioSpace in an email.
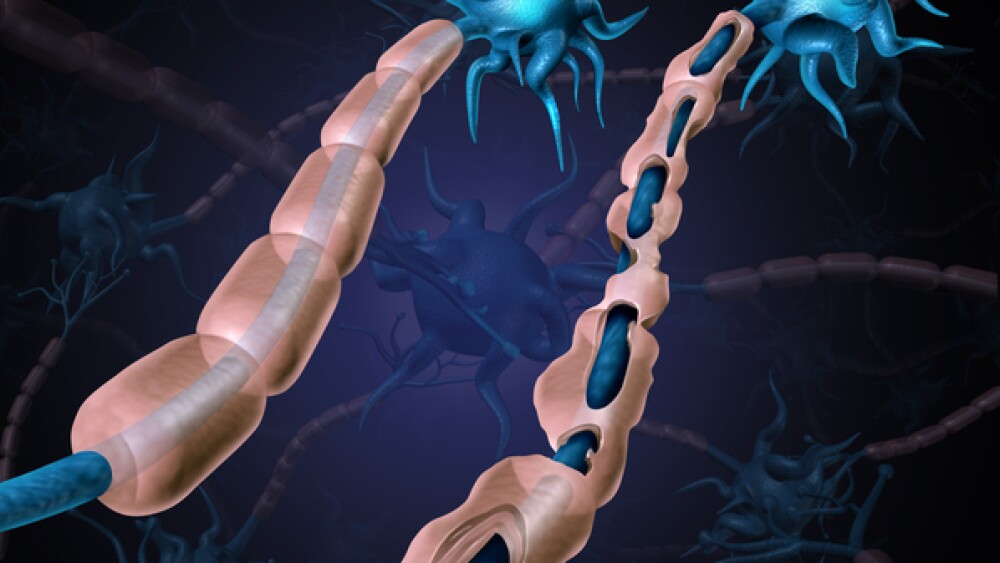
An international research team, including Greig, recently received funding to develop a treatment that targets excitotoxicity, a process that harms nerve cells in people living with MS. By blocking this process, the researchers hope to encourage the body to rebuild myelin—the protective coating around nerves damaged in MS—and improve nerve recovery. Greig explained that should human trials validate the drug, it would be revolutionary in its ability to effectively reverse the disease.
“Clearly, this is a dream scenario, but our pre-clinical data support this as a real possibility,” he said. “Alternatively, it may be that the nerve damage already sustained cannot be repaired even by remyelination, but reparation of the damaged myelin will prevent further neurodegeneration—thus ‘holding’ patients at an early ‘physically OK’ stage of the disease, as soon as they are diagnosed.”
The research is currently in the final preclinical stages of validation. According to Greig, the team has funding to get through to IND-enabling studies. Beyond this, they are investigating all approaches to financing clinical trials, including seeking private investment and presenting their research to pharmaceutical companies.
Back at ECTRIMS, University of Cambridge researchers presented Phase II clinical trial results indicating that a combination of metformin and clemastine showed potential to repair myelin. Previous evidence from animal studies suggested that metformin enhances the effect of clemastine on myelin repair, but until now, the two drugs had never been tested together in people.
“My instinct is that we are on the brink of a new class of treatments to stop MS progression,” Nick Cunniffe, a clinical lecturer in neurology at the University of Cambridge, who led the CCMR-Two trial, said in an article published on the school’s research page, “and within the next decade we could see the first licensed treatment that repairs myelin and improves the lives of people living with MS.”