Researchers at the Earle A. Chiles Research Center have successfully shrunk a woman’s pancreatic cancer tumors using a novel immunotherapy.
The medical community has reveled in cancer treatment breakthroughs lately, with new research making headlines weekly. Generating traction in this week’s news, researchers at the Earle A. Chiles Research Center within the Providence Cancer Institute of Oregon have successfully shrunk a woman’s pancreatic cancer tumors using a novel immunotherapy. The findings were published in the New England Journal of Medicine.
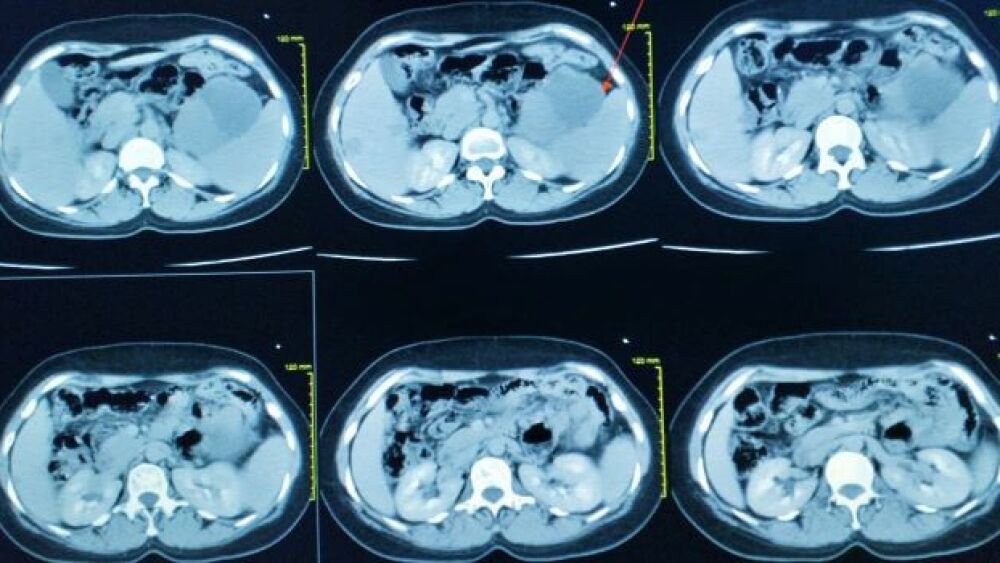
While the research is merely proof-of-concept at this phase, excitement is warranted. Participant one, Kathy Wilkes, received the one-time treatment as an alternative to traditional chemotherapy, in hopes of seeing better results. In her case, surgery, radiation and chemotherapy did little to slow the cancer’s spread, which had migrated from her pancreas to her lungs. In an interview published in the Associated Press, Wilkes explained her choice to try an experimental option.
“I knew that regular chemotherapy would not save my life and I was going for the save,” she said.
The tumors showed an overall partial response of 72% and no signs of regrowth six months after infusion treatment. Reassuringly, the engineered T cells accounted for 2% of all T cells circulating in the patient’s blood at the six-month mark.
The treatment involves taking T cells, which act as the body’s first line of defense and reprogramming them to identify the KRAS G12D mutation in tumor cells. The mutant protein within cancer cells is what causes rampant proliferation and metastasis. Typically, the mutation evades the immune system. With the genetic modification, the cancer cells are revealed to and killed by the T cells. Healthy cells remain safe from T cell attack. This method has been termed T cell receptor (TCR) therapy.
Eric Tran, a researcher at Oregon’s Providence Cancer Insitute, commented on the findings, saying that Wilkes’positive response “provides [him] with optimism that we’re on the right track.” Tran went on to say, “we’re talking about the chance to distinguish tumor cells from non-tumor cells in a way that we never could before.”
According to the American Cancer Society, pancreatic cancer accounts for 7% of all cancer deaths. Survival rates vary depending on whether the cancer has spread but the 5-year relative survival rate averages at 11%. Pancreatic cancer has a reputation for being difficult to treat, leaving a diagnosed patient to choose between traditional standard-of-care or entering experimental treatments.
An article in the New York Times about the treatment quotes Dr. William Jarnagin, an esteemed doctor at the Memorial Sloan Kettering Cancer Center who is not involved in this study as saying, “Our treatments are not doing the job.”
In the past, CAR-T therapy has been tried and failed as a potential pancreatic cancer treatment, despite the method’s success against other cancer forms. Scientists attribute this exception to the fact that solid tumors don’t display a warning marker on the tumor cell surface.
Additional research for TCR therapy is needed to evaluate the treatment’s potential. Before Wilkes, a patient zero was given the infusion therapy without showing any response. The institute’s researchers are now challenged with finding out why one patient responded while another did not, along with any other roadblocks that may arise. All in all, this announcement indicates that the fight against pancreatic cancer is ongoing.