Keytruda (pembrolizumab) hit one of the coprimary endpoints early in the Phase III KEYNOTE-177 clinical trial for a highly mutating form of colorectal cancer.
Merck’s checkpoint inhibitor Keytruda (pembrolizumab) hit one of the coprimary endpoints early in the Phase III KEYNOTE-177 clinical trial for a highly mutating form of colorectal cancer.
The trial is evaluating the drug in patients with microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR) unresectable or metastatic colorectal cancer. Interim analysis by an independent Data Monitoring Committee (DMC) found that Keytruda alone showed a statistically significant and clinically meaningful improvement in progression-free survival (PFS) compared to chemotherapy. The chemotherapy was investigator’s choice of mFOLFOX6 or FOLFIRI, with or without bevacizumab (Roche’s Avastin) or cetuximab (Eli Lilly’s Erbitux).
The other dual primary endpoint is overall survival. The DMC recommended the trial continue without changes to evaluate OS.
“These head-to-head data with Keytruda are the first time a single-agent, anti-cancer therapy, and particularly an anti-PD-1 monotherapy, achieved a statistically significant improvement in progression-free survival over chemotherapy, including the current standard of care regimen of mFOLFOX6 plus bevacizumab, in patients with MSI-H colorectal cancer,” said Roy Baynes, senior vice president and head of global clinical development, chief medical officer, Merck Research Laboratories.
The National Cancer Institute defines microsatellite instability (MSI) as changes in the DNA of certain cells, such as cancer cells, where the number of repeats of microsatellites——short, repeated DNA sequences—is different from the number of repeats in the inherited DNA. Researchers believe microsatellite instability is caused by a problem in the ability to fix mistakes made when DNA is copied in the cell. MSI is also called mismatch repair deficient (dMMR). About 10 to 15% of colorectal cancer tumors that are tested are either MSI-H or dMMR.
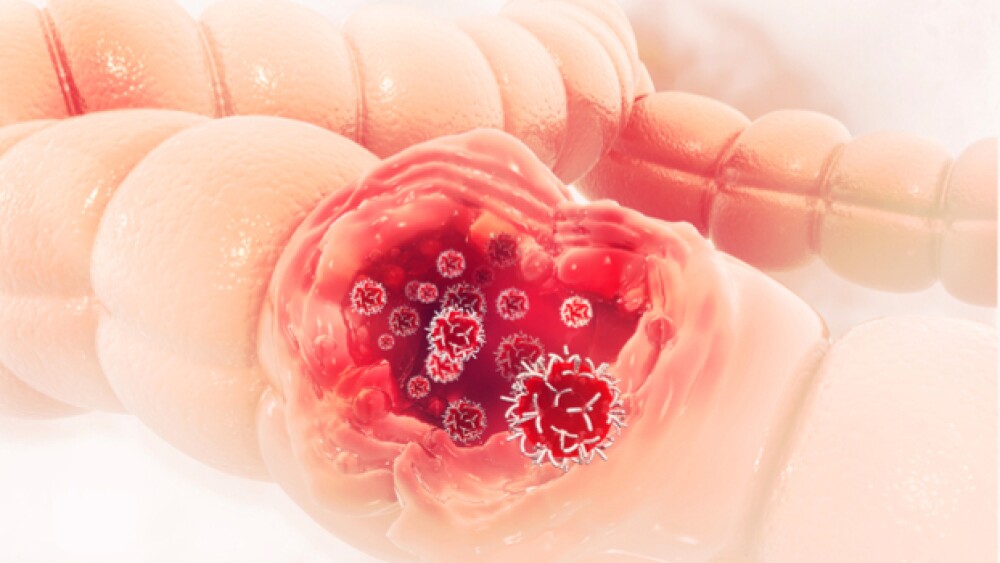
Cancers that begin in the colon or rectum are colorectal cancer and are classified as colon cancer or rectal cancer depending on the origin. There are about 850,000 new cases of colorectal cancer and 880,000 deaths from the disease around the world in 2018. In the U.S., there are about 105,000 new cases each year of colon cancer and more than 43,000 new cases of rectal cancer, causing more than 53,000 deaths combined in 2020. The five-year survival rates for advanced and metastatic colon cancer and rectal cancer are estimated to be 14% and 15%, respectively.
Keytruda is projected to become the world’s top-selling drug by about 2023. That title is currently held by AbbVie’s Humira, but will be losing patent protection and facing competition in 2023. Keytruda is projected to bring in $22.5 billion in revenue by 2025. In 2019, Keytruda global sales grew 55% to $11.1 billion.
Keytruda is approved for more than 20 cancer indications in the U.S. and racks up more on a fairly regular basis. Just some of those indications are melanoma, non-small cell lung cancer, head and neck cancer, classical Hodgkin Lymphoma, primary mediastinal large B-cell lymphoma, urothelial carcinoma, microsatellite instability-high (MI-H) cancer, gastric cancer, esophageal cancer and others.
Keytruda is involved in more than 1,200 clinical trials as a monotherapy or in combinations.
Of today’s trial, Baynes added, “These data in the first-line treatment setting provide further evidence of the benefits of Keytruda monotherapy in patients whose tumors are MSI-H or dMMR. We look forward to sharing these data as quickly as possible with the medical community and regulatory authorities.”