The FDA’s latest approval for Darzalex is based on results from the Phase III CASSIOPEIA trial that showed the addition of Darzalex to VTd before and after ASCT resulted in deeper responses in patients with the blood cancer.
Janssen’s Darzalex continues to impress the U.S. Food and Drug Administration (FDA). The regulatory agency awarded the drug in combination with bortezomib, thalidomide and dexamethasone (VTd) for newly diagnosed patients with multiple myeloma who are eligible for autologous stem cell transplant (ASCT).
The FDA’s latest approval for Darzalex is based on results from the Phase III CASSIOPEIA trial that showed the addition of Darzalex to VTd before and after ASCT resulted in deeper responses in patients with the blood cancer. That was indicated by the higher stringent complete response rate and improved progression-free survival compared to VTd alone, Janssen, a division of Johnson & Johnson said. The latest approval for Darzalex was granted under Priority Review.
“The Darzalex clinical development program has led to many important firsts, but more importantly, it has generated key insights and understanding into the biology and treatment of multiple myeloma,” Craig Tendler, vice president of clinical development and global medical affairs in oncology at Janssen Research & Development, said in a statement. “Today’s milestone marks the seventh FDA approval in less than four years for Darzalex, and the third for newly diagnosed patients.”
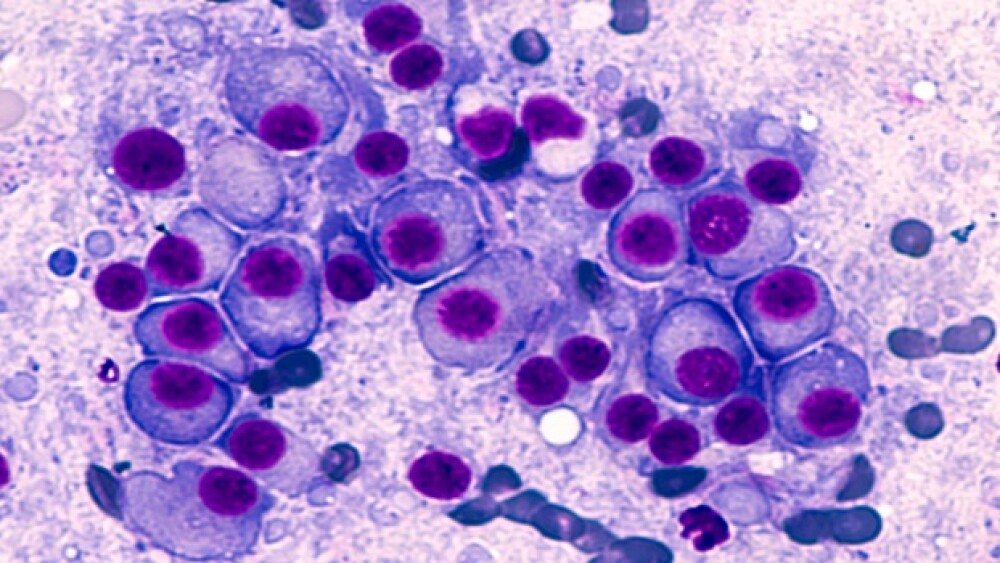
Multiple myeloma is an incurable blood cancer that affects plasma cells found in the bone marrow. In 2019, it is estimated that 32,110 people will be diagnosed and 12,960 will die from the disease in the United States. Autologous stem cell transplants, which uses the patient’s own stem cells, in combination with chemotherapy are a common treatment for multiple myeloma.
Earlier this year, a split-dosing program for Darzalex (daratumumab), was approved in combination with bortezomib, melphalan and prednisone for patients with newly diagnosed multiple myeloma who are ineligible for autologous stem cell transplant. It is also approved in combination with lenalidomide and dexamethasone, or bortezomib and dexamethasone, for MM who have had at least one previous therapy; and in combination with pomalidomide and dexamethasone for patients with MM who’ve had at least two previous treatments, including lenalidomide and a proteasome inhibitor. In June, Darzalex was approved in combination with lenalidomide and dexamethasone for the treatment of patients with newly diagnosed multiple myeloma who are ineligible for autologous stem cell transplant.
Tendler added that Janssen’s work with Darzalex is ongoing. He said the company is committed to discovering and developing innovative treatments like Darzalex for the benefit of patients facing a multiple myeloma diagnosis.”
Results from the first part of the CASSIOPEIA trial showed that the primary endpoint of sCR rate post-consolidation was significantly higher in the Darzalex-VTd arm compared to VTd alone, 29% to 20% respectively. The addition of Darzalex to VTd at a median follow-up of 18.8 months resulted in a 53%reduction in the risk of disease progression or death compared to VTd alone, the data showed.
The combination of Darzalex-VTd also increased the rate of complete response or better compared to VTd alone, 39% vs. 26%, Janssen said.
Philippe Moreau, principal investigator of the trial and head of the Hematology Department at the University Hospital of Nantes in France, said the CASSIOPEIA study is one of the largest transplant studies ever conducted in multiple myeloma and the largest with Darzalex. The data from the Phase III study shows the addition of Darzalex to VTd before and after transplant “markedly increased depth of response compared to VTd alone for patients with newly diagnosed multiple myeloma.”
The most frequent adverse reactions in the Darzalex-VTd group were infusion reactions, nausea, pyrexia, upper respiratory tract infection and bronchitis. In the Darzalex-VTd combination arm, infusion-related reactions occurred in 35% of patients.