The platform, called LOCOcyte™, is a cytokine delivery platform that is made of polymer-encapsulated human ARPE-19 cells that produce natural cytokines.
An immuno-therapeutic platform technology – essentially a cytokine factory – that eradicates 100% of intraperitoneal tumors has been developed by researchers at Rice University and licensed exclusively to Avenge Bio, Inc. It appears to have the potential to dramatically improve prognosis for ovarian cancer patients.
There is a caveat, however. These results have, so far, only been demonstrated in animal models. This study, published in the peer-reviewed journal Science Advances, establishes proof of concept.
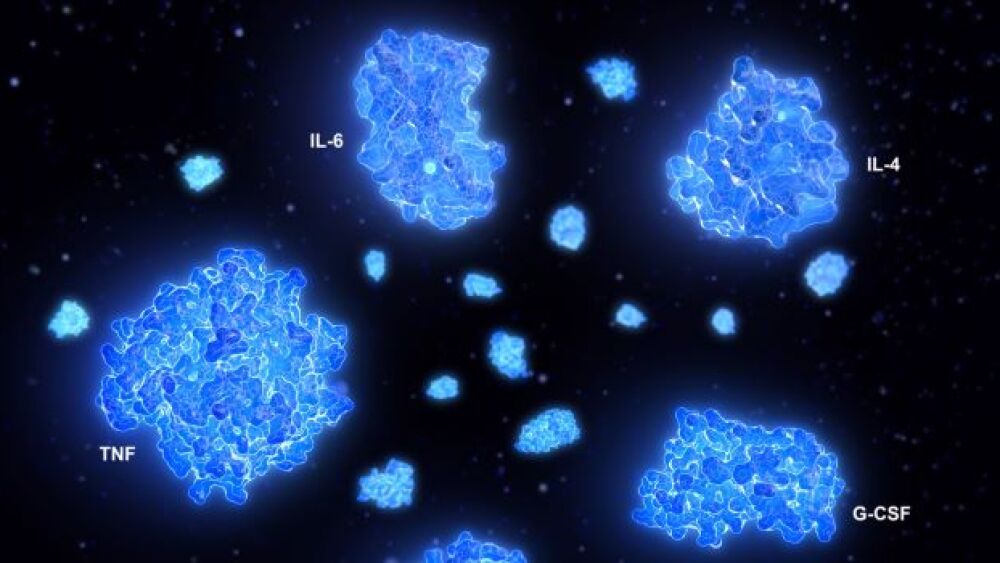
The platform, called LOCOcyte™, is a cytokine delivery platform that is made of polymer-encapsulated human ARPE-19 cells that produce natural cytokines. When the encapsulated cells are delivered next to the tumors, they produced interleukin-2 (IL-2) and eradicated the peritoneal tumors in mice with ovarian and colorectal cancer. Both a local and systemic immune response was created. The study showed no systemic toxicity and allowed both spatial and temporal control.
Similar outcomes in terms of efficacy and safety were found when LOCOcyte™ was administered in non-human primate studies, where it elicited T cell responses indicative of therapeutic efficacy without toxicity. If LOCOcyte™ is effective in humans, as the researchers expect, it holds the promise of replacing the toxic, high-dosage infusions associated with cytokine therapy today.
“This platform has the potential to be a new modality for ovarian cancer patients,” research team leader Omid Veiseh, Ph.D., assistant professor of bioengineering at Rice University and a founder of Avenge Bio, told BioSpace. “We believe it will change the paradigm of how people deliver immunotherapy.
“Traditionally, most therapies are delivered intravenously, but there are so many immune cells in the blood that patients often get off-target side effects, and very little cytokine actually makes it to the tumor site. But here, we are reversing the concentration gradient and, instead, creating high cytokine concentrations at the tumor site without disrupting the immune cells in the blood,” he said.
Ovarian cancer is a notoriously difficult cancer to treat, partially because it often isn’t discovered until it has reached advanced stages. Approximately 70% of ovarian cancer patients will experience a recurrence of the cancer, which is frequently fatal. The Centers for Disease Control & Prevention lists ovarian cancer number five in terms of causes of cancer deaths among women in the U.S., affecting 6.9 per 100,000 women.
Recombinant IL-2, which is FDA-approved to treat ovarian cancer has a half-life measured in minutes. To compensate, it is administered in high doses that cause severe side effects, including vascular leak syndrome, which can damage the major organs and trigger the development of antidrug antibodies.
Native IL-2, which LOCOcyte™ creates, doesn’t cause those side effects. It, however, is unstable. Researchers, therefore, concentrated upon finding better ways to deliver recombinant IL-2. Controlled release formulations, mRNA-based formulations and IL-2 analogs, conjugates and fusion proteins have been developed to minimize dose-related toxicities. Despite promising results of those approaches, “An approach to simultaneously account for the short lifetime, maintain the full biological activity, and limit systemic toxicity of IL2 remains elusive,” Veiseh and colleagues wrote in the paper, “Clinically translatable cytokine delivery platform for eradication of intraperitoneal tumors.”
Local, intraperitoneal (IP) administration seems a promising way to side-step what he called the activity-toxicity tradeoff. That’s because, as the researchers explained, “The peritoneal cavity is separated from the systemic circulation by the peritoneal wall,” thereby compartmentalizing the infusion of IL-2 in a way that is not feasible with intravenous or subcutaneous administration. That also means a smaller dose is needed.
The value of local administration was shown in a Phase II trial conducted in 2010 at the University of Pittsburgh by Anda Vlad and colleagues. That trial involved 24 ovarian cancer patients who had platinum-resistant tumors. The overall 25% response rate included four complete remissions and two partial remissions, and a highly favorable safety profile. Side effects were significantly reduced because of an approximate 100-fold reduction in the local concentration of IL-2 when the therapy was administered into the intraperitoneal cavity rather than in the bloodstream.
The therapeutic platform developed by Veiseh and colleagues offers a modular way to deliver IL-2 without requiring stimulation from the host while producing natural cytokines within the fluid tumor microenvironment. The platform was designed to function for only 30 days, thus limiting side effects.
In the study of the lead compound, AVB-001, 100% of mice with advanced ovarian cancer showed a significant tumor burden reduction after 30 days, compared to controls. Specifically, mice receiving the lowest dosage showed a 3.2-fold reduction in tumor burden. Those receiving a 10-times higher dosage experienced 147-fold less tumor burden than controls. These tests were repeated twice, involving a total of 20 mice.
The next step is to embark upon a Phase I clinical trial to identify the optimum dosage.
“We have thought about translation from the beginning of the project and have had several meetings with the FDA,” Veiseh said. “In addition, we have licensed this technology to Avenge Bio, which is moving forward to human clinical trials in late 2022. We are also planning to test this system in other cancer models such as lung cancer, where we would administer the capsules in the pleural cavity. Other cancers, such as breast cancer and melanoma, potentially could also benefit from local administration of immunotherapeutic molecules.”
Avenge Bio closed a $45 million Series A funding round in January.