The researchers identified a group of centyrins that blocked the action of five toxins generated by Staphylococcus aureus, the bacteria that causes Staph infections.
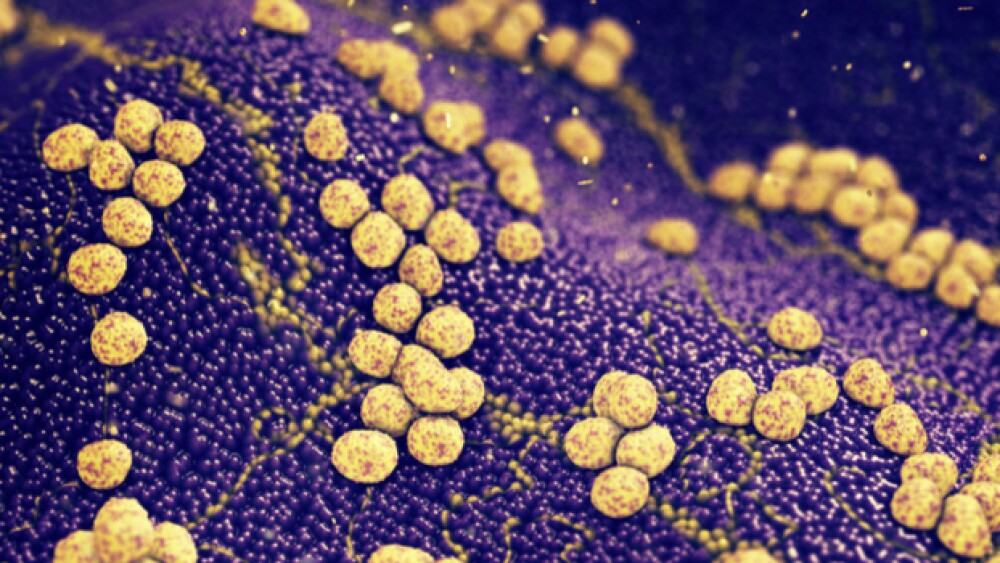
Staphylococcus aureus infection.
Researchers at New York University School of Medicine and Janssen Research & Development, a Johnson & Johnson company, have developed a new class of engineered proteins that may help fight the bacteria that cause Staph infections.
The results of a five-year research partnership were published in the journal Science Translational Medicine. “To our knowledge, this is the first report showing that proteins called centyrins can potentially block the effects of severe S. aureus bacterial infections in mice, and in human cell experiments,” stated lead author Victor Torres, associate professor in the Department of Microbiology at NYU Langone Health.
The researchers identified a group of centyrins that blocked the action of five toxins generated by Staphylococcus aureus, the bacteria that causes Staph infections. These five toxins are used by the bacteria to evade the human immune system. The centyrins don’t destroy the germs but take away their ability to thrive. This new approach has the potential to deal with antibiotic resistance.
A January 2018 report by the World Health Organization (WHO)’s Global Antimicrobial Surveillance System (GLASS), found widespread antibiotic resistance among 500,000 people with suspected bacterial infections in 22 countries. The most commonly reported bacteria resistant to antibiotics were Staphylococcus aureus, Escherichia coli, Klebsiella pneumoniae, and Streptococcus pneumoniae, followed by Salmonella species.
Marc Springer, director of WHO’s Antimicrobial Resistance Secretariat, stated at the time, “The report confirms the serious situation of antibiotic resistance worldwide. Some of the world’s most common—and potentially most dangerous—infections are proving drug-resistant. And most worrying of all, pathogens don’t respect national borders. That’s why WHO is encouraging all countries to set up good surveillance systems for detecting drug resistance that can provide data to this global system.”
About a third of all people around the world are carriers of S. aureus, typically without symptoms. But in people with weakened immune systems, S. aureus can cause serious, life-threatening infections in the lung, heart, bone or bloodstream. Staph infections are a serious problem in hospitals, where because of widespread use of antibiotics, especially methicillin, methicillin-resistant S. aureus (MRSA) infections cause 11,000 deaths in the U.S. annually.
In 1998, researchers, including NYU’s Shohei Koide, discovered a class of proteins that came from fibronectin type III (FN3) protein subunits. They were originally classified as monobodies and investigated as cancer treatments by Janssen researchers. Centyrins are FN3 “scaffolds” optimized for drug development, and eventually, Janssen used them to as anti-toxins.
The toxins produced by S. aureus, such as leucocidin AB, which was identified by Torres’ laboratory, drill holes in immune cells, killing them before they can kill the bacteria. They also drill into red blood cells, flooding bacteria with nutrients.
The researchers in this study used molecular techniques and automation to change a single parental centyrin, which created a trillion slightly modified centyrins. They screened the library and found 209 centyrins that bind to pieces of one of the five major S. aureus leukotoxins. In human cells, they found that the ones that bound the tightest could prevent the toxins from attaching and destroying the cells they would otherwise drill into.
Dosing mice with toxic levels of LukED S. aureus toxin, they also dosed some of the mice with the SM1S26 centyrin. The mice who didn’t receive the centyrin died, while those who did receive it lived. Even in cases where the mice received centyrin four hours after live S. aureus infection, half of the infected animals survived compared to none in the control group of infected mice.
The team is now working to develop biologics that combine centyrins with anti-staphylococcal monoclonal antibodies in a new class of proteins called MABtyrins.
“One of the most exciting aspects of this work is that scientists may be able to pick their pathogen, and then easily generate a vast, cost-effective library of centyrins shaped to interfere with the disease process at hand,” Torres stated. “It’s bigger than one experimental treatment.”