In a study published online in Science today, scientists at UCSF QBI and the Department of Microbiology at Icahn School of Medicine at Mount Sinai (ISMMS) reported data showing the promise and potential of Aplidin® (plitidepsin), a drug approved by the Australian Regulatory Agency for the treatment of multiple myeloma, against SARS-CoV-2, the virus that causes COVID-19
SAN FRANCISCO, Jan. 25, 2021 (GLOBE NEWSWIRE) -- In a study published online in Science today, scientists at UCSF QBI and the Department of Microbiology at Icahn School of Medicine at Mount Sinai (ISMMS) reported data showing the promise and potential of Aplidin® (plitidepsin), a drug approved by the Australian Regulatory Agency for the treatment of multiple myeloma, against SARS-CoV-2, the virus that causes COVID-19. Specifically, plitidepsin demonstrated antiviral activity that was 27.5-fold more potent against SARS-CoV-2 in vitro than remdesivir, a drug that received FDA emergency use authorization in 2020 for the treatment of COVID-19. In addition, in two preclinical models of COVID-19, plitidepsin showed a 100-fold reduction in viral replication in the lungs and demonstrated an ability to reduce lung inflammation. Furthermore, in a separate publication in bioRxiv, the researchers, in collaboration with Greg Towers and Clare Jolly at University College London in London, England, shared additional in vitro data demonstrating comparable anti-viral activity of plitidepsin in the newly identified b.1.1.7 variant mutant strain of SARS-CoV-2 when compared to the original SARS-CoV-2 strain. Additionally, they found plitidepsin to be ~100 times more potent than remdesivir in human epithelial cells.
The studies were led by the laboratories of Nevan Krogan, Ph.D., Director of the Quantitative Biosciences Institute (QBI) at the School of Pharmacy at UC San Francisco, Senior Investigator at Gladstone Institutes, and Adolfo García-Sastre, Ph.D., Professor in the Department of Microbiology and Director of the Global Health and Emerging Pathogens Institute of ISMMS in New York, among others.
“From the start, our scientific investigation at QBI’s Coronavirus Research Group (QCRG) was to research where and how the SARS-CoV-2 virus was co-opting its human host to thrive, survive and become deadly,” said Dr. Krogan. “That research led us to a biologic pathway, eukaryotic translation machinery, where inhibition of this pathway showed significant antiviral activity in cell culture. One of the promising agents that arose from our screen of drugs that inhibit this pathway was plitidepsin. The preclinical data published today showing increased potency compared to remdesivir, and in conjunction with recent early clinical data showing promise in COVID-19 patients as reported by the drug’s manufacturer, highlight plitidepsin should be further evaluated as a COVID-19 therapy. Additionally, this further validates our prospective and novel approach of looking first at host mechanisms that permit the virus to wreak havoc. By targeting host factors that enable or facilitate disease, we have the potential to have a more far-reaching impact in drug development. In this case, SARS-CoV-2 and its mutant strains, and possibly other viruses that leverage the same pathway may also be susceptible to the same therapeutic agents that inhibit this virus-host interaction.”
The research studies showed that the anti-SARS-CoV-2 activity of plitidepsin was potent in human cells, with an IC90 of 0.88 nM, which was a 27.5-fold more potent antiviral than remdesivir tested in the same cell line. In addition, the antiviral effect of plitidepsin was tested in an established model of human lung cells, which showed that treatment with plitidepsin inhibited SARS-CoV-2 replication with an IC90 of 3.14 nM and a selectivity index of 40.4, suggesting that plitidepsin has potent antiviral activity in primary human lung cells. The researchers also tested the synergy between plitidepsin and remdesivir, given remdesivir’s use as part of the current standard of care for the treatment of COVID-19. In vitro data suggests that plitidepsin has an additive effect with remdesivir and would be a potential candidate to be considered in a combined therapy.
Dr. García-Sastre added, “The ongoing SARS-CoV-2 pandemic has created the immediate need for antiviral therapeutics that can be moved into the clinic urgently. This led us to screen clinically approved drugs with established bioavailability, pharmacokinetics and safety profiles. Our previous study of the SARS-CoV-2 interactome led us to the eEF1A eukaryotic translation pathway as a druggable target with the potential for potent inhibition of SARS-CoV-2. Furthermore, this pathway has been previously described to be an important host factor for the replication of many viral pathogens, including influenza virus and RSV suggesting its pan-antiviral targeting potential. These studies have only been possible by the combined efforts and expertise of the multiple academic research groups that are co-authors in the published study. We have also been doing these studies in close collaboration with PharmaMar, the company that first isolated the potent eEF1A inhibitor plitidepsin/ Aplidin® from a sea organism.”
“Plitidepsin is an extremely potent inhibitor of SARS-CoV-2, but its most important strength is that it targets a host protein rather than a viral protein,” said Kris White, Ph.D., Assistant Professor in the Department of Microbiology of Icahn School of Medicine at Mount Sinai (ISMMS), who was a corresponding author on the Science paper. “This means that if plitidepsin is successful in the treatment of COVID-19, the SARS-CoV-2 virus will be unable to gain resistance against it through mutation, which is a major concern with the spread of the new U.K. and South African variants.”
About QBI: The Quantitative Biosciences Institute (QBI) is a University of California organized research unit reporting through the UCSF School of Pharmacy. QBI fosters collaborations across the biomedical and the physical sciences, seeking quantitative methods to address pressing problems in biology and biomedicine. Motivated by problems of human disease, QBI is committed to investigating fundamental biological mechanisms, because ultimately solutions to many diseases have been revealed by unexpected discoveries in the basic sciences. Learn more at qbi.ucsf.edu.
About UCSF: The University of California, San Francisco (UCSF) is exclusively focused on the health sciences and is dedicated to promoting health worldwide through advanced biomedical research, graduate-level education in the life sciences and health professions, and excellence in patient care. UCSF Health, which serves as UCSF’s primary academic medical center, includes top-ranked specialty hospitals and other clinical programs, and has affiliations throughout the Bay Area. Learn more at ucsf.edu or see our Fact Sheet.
About the Mount Sinai Health System: The Mount Sinai Health System is New York City's largest academic medical system, encompassing eight hospitals, a leading medical school the Icahn School of Medicine, and a vast network of ambulatory practices throughout the greater New York region. Mount Sinai is a national and international source of unrivaled education, translational research and discovery, and collaborative clinical leadership ensuring that we deliver the highest quality care—from prevention to treatment of the most serious and complex human diseases. Learn more at mountsinai.org.
About Gladstone Institutes: To ensure our work does the greatest good, Gladstone Institutes focuses on conditions with profound medical, economic, and social impact—unsolved diseases. Gladstone is an independent, nonprofit life science research organization that uses visionary science and technology to overcome disease. It has an academic affiliation with UC San Francisco. Learn more at gladstone.org.
Authorship and funding: This work was funded by grants from the National Institute of Mental Health and the National Institute of Allergy and Infectious Diseases, both part of the National Institutes of Health; the Defense Advanced Research Projects Agency; the Center for Research for Influenza Pathogenesis; the Centers of Excellence for Influenza Research and Surveillance of the National Institute of Allergy and Infectious Diseases; the Centers of Excellence for Integrative Biology of Emerging Infectious Diseases of the Agence Nationale de la Recherche (France); F. Hoffmann-LaRoche AG; Vir Biotechnology, Centre for Integrative Biological Signalling Studies (CIBSS), European Research Council (ERC) and QCRG philanthropic donors. Shokat is a Howard Hughes Medical Institute investigator. A complete list of authors and full funding information is available in the Science paper.
Media Contacts
| UCSF QBI | UCSF |
| Sylvia Wheeler, Wheelhouse LSA | Pete Farley, UCSF Office of Communications |
| swheeler@wheelhouselsa.com | peter.farley@ucsf.edu |
| 415-317-3781 | |
| Aljanae Reynolds, Wheelhouse LSA | Mount Sinai Health System |
| areynolds@wheelhouselsa.com | Lucia Lee, Mount Sinai Communications |
| lucia.lee@mountsinai.org | |
| 917-837-8914 | |
| Gladstone Institutes | Icahn School of Medicine at Mount Sinai |
| Julie Langelier, Gladstone Communications | Marlene Espinoza-Moraga, PhD |
| Julie.langelier@gladstone.ucsf.edu | marlene.espinozamoraga@mssm.edu |
| 415-734-5000 | 212-241-9812 |
Photos accompanying this announcement are available at
https://www.globenewswire.com/NewsRoom/AttachmentNg/f42dab31-fb28-4b44-a755-9578899e1c37
https://www.globenewswire.com/NewsRoom/AttachmentNg/ea32d7c0-2aed-4541-a530-764bb2cb74dd
https://www.globenewswire.com/NewsRoom/AttachmentNg/35a69fe5-e473-4fcc-bada-7512ce436896
https://www.globenewswire.com/NewsRoom/AttachmentNg/6638f44e-4df0-4043-8b29-e013b2519c0e
A video accompanying this announcement is available at https://www.globenewswire.com/NewsRoom/AttachmentNg/97334c89-f27f-4029-be38-63a1d75bb46a
Aplidium albicans
Aplidin was extracted from Aplidium albicans, a sea squirt found off the coast of Spain
Aplidium albicans
Aplidin was extracted from Aplidium albicans, a sea squirt found off the coast of Spain
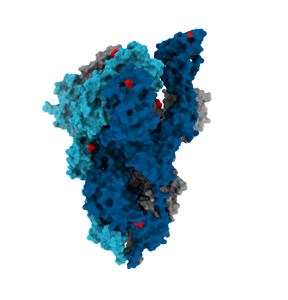
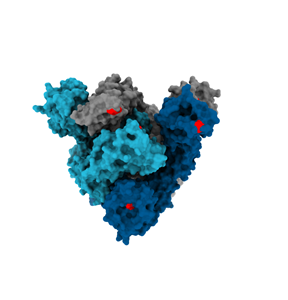
Coronavirus Spike Protein
Structure of the coronavirus Spike protein (light blue, dark blue, and grey), which is essential for viral entry into human cells, adorned with the mutations (red, 8 in Spike) in the United Kingdom coronavirus variant.
Coronavirus Spike Protein