Every week there are numerous scientific studies published. Here’s a look at some of the more interesting ones.
Every week there are numerous scientific studies published. Here’s a look at some of the more interesting ones.
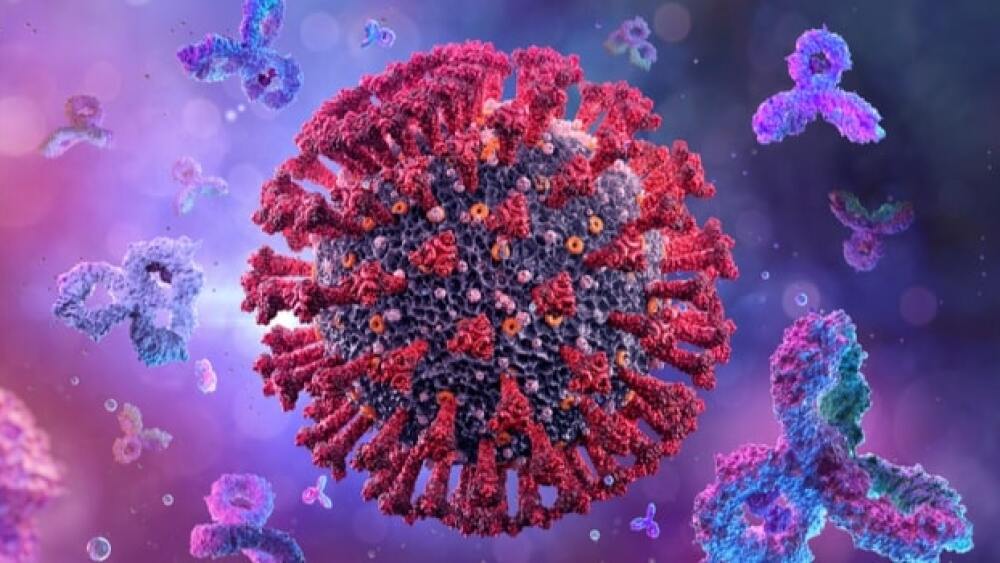
Post-COVID Infection, The Older You Are the More Antibodies You Have
Researchers at the University of Montreal found that people over the age of 50 who recovered from a mild case of COVID-19 had more antibodies against the virus than younger people. The research also found that people who received the Pfizer-BioNTech or AstraZeneca-Oxford COVID-19 vaccines had significantly higher antibody levels than people who recovered from infections, and those antibodies were effective against the Delta variant. The research was published in Scientific Reports.
“Everyone who had been infected produced antibodies, but older people produced more than adults under 50 years of age,” said Jean-Francois Masson, who co-led the research.
They found that antibodies generated after an infection by the original wildtype Wuhan strain of the virus also reacted to various variants, namely Beta (South Africa), Delta (India) and Gamma (Brazil), but there was a reduction of antibodies by 30% to 50%.
“But the result that surprised us the most was that antibodies produced by naturally infected individuals 50 and older provided a greater degree of protection than adults below 50,” said Joelle Pelletier, who co-led the research. “This was determined by measuring the antibodies’ capacity to inhibit the interaction of the Delta variant’s spike protein with the ACE-2 receptor in human cells, which is how we become infected. We didn’t observe the same phenomenon with the other variants.
Galectin-1 Associated with an Increased Risk of Type 2 Diabetes
Investigators at the University of Gothenberg linked elevated levels of the protein galectin-1 with an increased risk of type 2 diabetes (T2D) approximately 18 years later. However, the protein appears to act as a protective factor for the kidneys in type 2 diabetics at high risk for diabetic nephropathy. In a general population, galectin-1 seems tied to an increased risk of T2D. But in patients with a subtype of diabetes that comes with an increased risk of kidney damage, patients with high galectin-1 levels seem to have less kidney damage. Part of the reasoning is that galectin-1 in the kidney is associated with inflammatory processes, while galectin-1 in fat (adipose) tissue seems associated with metabolic processes. Galectin-1 is expressed by fat cells and other cells but is involved in regulating inflammation and the function of fat cells.
New Findings on Cellular Aging
A study out of the University of Montreal Hospital Research Centre (CRCHUM) demonstrated that cellular senescence, which is when aging cells no longer divide, but are not dead, is caused by irreversible damage to the genome. It was previously thought that it was the result of telomere erosion. Telomeres are the caps at the end of chromosomes, and they shorten each time a cell divides. Once telomeres get too short, they inform the cell to stop dividing, resulting in senescence. In their research, they were able to ensure that all telomeres of a population of cells became dysfunctional, then used imaging equipment to observe what was happening inside the cells in real time. They found that before entering senescence, the cells divided one last time, but that cell division caused by telomere dysfunction was so unstable that it created genetic defects—leading them to conclude that senescent cells have an abnormal genome. And that these abnormalities could result in many diseases of aging, such as cancer.
Missing Molecule in Red Blood Cells Tied to Type 2 Diabetes Vascular Damage
People with type 2 diabetes are at increased risk of cardiovascular disease, including damaged blood vessels, which can lead to life-threatening heart attacks and stroke. But how this happens was not well understood. Now, researchers with the Karolinska Institute found that a missing molecule in red blood cells (RBC) causes the vascular damage. It has been well understood that RBCs become dysfunctional in type 2 diabetes and act as mediators of vascular problems. The team found that levels of microRNA-210 was significantly decreased in RBCs in type 2 diabetes compared to RBCs in 32 healthy patients. Micro-RNAs are in a group of molecules that act as regulators of vascular function in diabetes and other diseases. The decrease in microRNA-210 caused changes in specific vascular protein levels, which impaired blood vessel endothelial cell function. They found that in laboratory assays, restoring microRNA-210 levels in RBCs prevented the development of vascular injury.
Fibrinogen Directly Causes Brain Inflammation
A study out of the University of South Florida (USF Health) found that soluble fibrinogen, which is converted into insoluble fibrin molecule that can accumulate toxically outside blood vessels in the brain, can directly cause neuron inflammation. They believe this may point to new therapeutics for neurodegenerative diseases such as Alzheimer’s or traumatic brain injury. Their findings showed that insoluble fibrin molecules are able to directly connect with neurons and cause an inflammatory reaction. They also observed that fibrinogen binds to two fibrinogen receptors on the surface of neurons called cellular prion protein (PrPC) and intracellular adhesion molecule-1 (ICAM-1). Fibrinogen is naturally produced in the liver and is found throughout the bloodstream. During blood clotting, it is converted by thrombin into fibrin, where it plays a key role in wound healing. Fibrinogen also interacts with astrocytes, neural immune cells also implicated in Alzheimer’s disease. Their research also found that by blocking the PrPC and ICAM-1 receptors on neuron cells, they decreased inflammation that led to neurodegeneration.
More Data Supports Role of Immune Dysfunction in Alzheimer’s Disease
Research is increasingly finding that microglia, specialized immune cells in the brain, and their dysfunction, are associated with Alzheimer’s disease. Researchers at Indiana University School of Medicine were studying a gene mutation found in Alzheimer’s patients. They found that deleting the gene, ABI3, in laboratory animals, significantly increased beta amyloid plaques in the brain and decreased the number of microglia around the plaques. In their mouse model, the mice with the deleted gene had increased plaque levels, increased brain inflammation, and indications of synaptic dysfunction, which is associated with learning and memory deficits. The deletion also disrupted the microglia’s ability to move, meaning they couldn’t move closer to plaques to try to remove them. Amyloid plaques are associated with Alzheimer’s disease.
“Our study provides the first in vivo functional evidence that the loss of ABI3 function may increase the risk of developing Alzheimer’s disease by affecting amyloid beta accumulation and neuroinflammation,” said Hande Karahan, postdoctoral fellow in medical and molecular genetics.