A research team led by Jessica A. Hamerman, PhD, at Benaroya Research Institute at Virginia Mason (BRI), has discovered a unique type of cell and its association with a life-threatening complication of viral and autoimmune diseases.
|
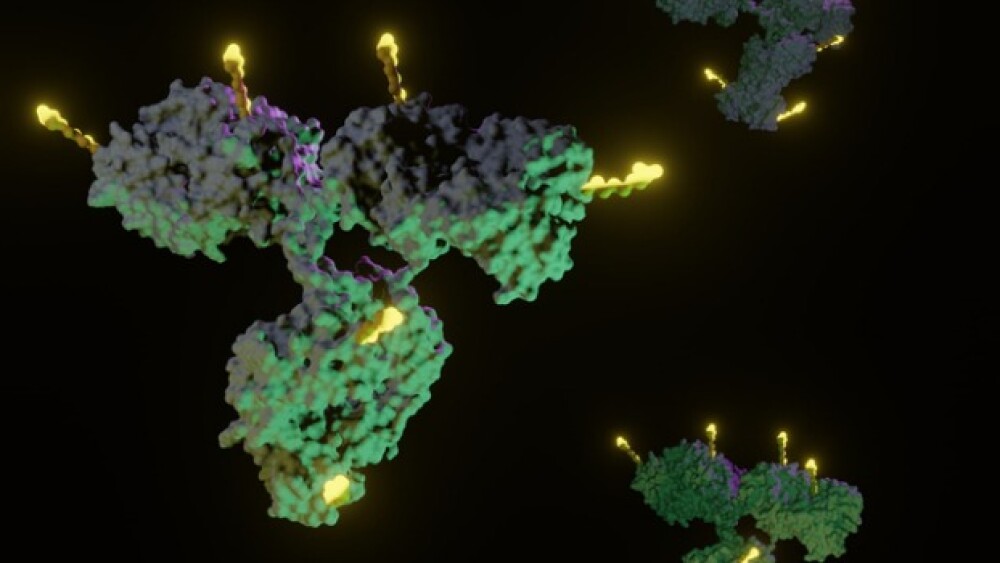
SEATTLE, /PRNewswire/ -- A research team led by Jessica A. Hamerman, PhD, at Benaroya Research Institute at Virginia Mason (BRI), has discovered a unique type of cell and its association with a life-threatening complication of viral and autoimmune diseases. The team's discovery, published in the journal Science, could lead to new treatments for a deadly form of inflammation in children with systemic juvenile idiopathic arthritis (SJIA), malaria and Kawasaki disease as well as patients with lupus. Macrophage activation syndrome, or MAS, is an inflammatory condition that leads to anemia, and people with the condition suffer persistent fevers, headaches, large lymph nodes and can, in severe cases, lead to organ dysfunction or death. Dr. Hamerman's team found a unique type of cell, which they termed "inflammatory hemophagocytes" (iHPCs), that eat red blood cells in MAS and malaria. The research team was able to show that the iHPCs develop under the influence of two specific proteins that recognize infection and are associated with autoimmune disease. "Our discovery demonstrates that if we interfere with the development of these iHPCs, we'll be able to treat MAS as well as other dangerous forms of anemia," Hamerman said. "We can draw a parallel between autoimmune or viral associated MAS and malaria. The same signals cause iHPCs and anemia in these diseases. In both cases, the iHPCs are 'eating' red blood cells and destroying them." "We were surprised by this discovery," Hamerman said. "Going into this project, we had some idea as to how the pathway worked, but we didn't anticipate that a particular type of macrophage would be involved in MAS." The team has been working on the project for about five years, Hamerman said. "Another thing that was really surprising to us is that we found these same cells causing anemia during infections – particularly in malaria," she said. According to Hamerman, next steps will involve collaborations with pediatricians and pediatric rheumatologists to look for iHPCs in the blood of children with autoimmune disease related anemia, as well as healthy individuals, with a goal of quickly identifying potential targets for treatments. Comparisons with blood samples infected by malaria are already under way, she said. Dr. Hamerman and her lab at BRI leverage multiple partnerships while focusing on the regulation of the innate immune response to pathogens with an emphasis on macrophages and dendritic cells. "For 20 years we've been leading and building collaborations to research the immune system, autoimmune diseases and immune-related diseases," said Jane Buckner, MD, president of BRI. "It's who we are and what we do." "And like every important scientific discovery, this one involved the hard work of many people," Buckner said. "Most of the work was done at BRI, but it also involved collaborations with other institutions in Seattle and around the country. We intend to continue working together so that we can accelerate translating discoveries into treatments for these life-threatening diseases."
SOURCE Benaroya Research Institute at Virginia Mason |