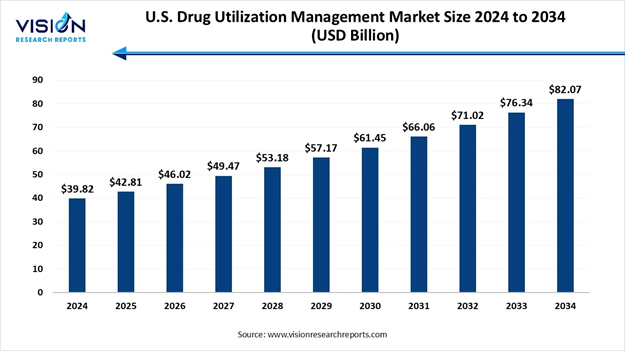
The U.S. drug utilization management market size was calculated at USD 39.82 billion in 2024 and is expected to grow steadily from USD 42.81 billion in 2025 to reach nearly USD 82.07 billion by 2034, expanding at a CAGR of 7.5% from 2025 to 2034, Study Published by Vision Research Reports.
The market growth is largely driven by increasing prescription drug spending, the broader implementation of value-based care models, and the growing use of advanced data analytics and AI-powered solutions to optimize medication utilization and minimize avoidable healthcare costs.
Note: This report is readily available for immediate delivery. We can review it with you in a meeting to ensure data reliability and quality for decision-making.
Preview the Report Before You Buy – Get Sample Pages 👉 https://www.visionresearchreports.com/report/sample/41416
What is Drug Utilization Management?
Drug utilization management (DUM) is a process which is a part of a human health plan. Drug utilization management helps in making sure that people are receiving the right type of drugs while also simultaneously making medicine more reasonable. Health plan firms, doctors, hospitals, and pharmacists share information and work together in order to support advanced medicine for people.
Drug utilization management programs, such as prior authorizations, step therapy, and quantity limits help to identify and deal with errors, lessen waste, improve safety and have medicine accessible by dropping costs. These types of programs are important for monitoring healthcare expenses, prompting patient care results and enhancing the overall quality of treatment. The most effective utilization management approaches concentrate on four main components, including risk minimization, quality assurance, patient education and in-depth review.
U.S. Drug Utilization Management Market Key Highlights
• By program type, the in-house segment captured the maximum market share of 66% in 2024.
• By program type, the outsourced segment is estimated to expand the fastest CAGR throughout the forecast period.
• By end-use, the PBMs segment registered the maximum market share of 38% in 2024.
• By end-use, the health plan provider/payors segment is seen to grow at the fastest rate during the forecast years.
What are the Key Growth Factors in the U.S. Drug Utilization Management Market?
The growth of the U.S. drug utilization management (DUM) market is driven by an increasing healthcare costs have spurred the need for strategies that optimize medication use and control expenditures. DUM techniques such as utilization review, prior authorization, and step therapy help healthcare organizations manage drug utilization efficiently, thus reducing unnecessary spending. Additionally, advancements in healthcare technology have enabled more sophisticated approaches to DUM, including the use of data analytics and electronic health records to monitor and improve prescribing patterns.
Regulatory initiatives aimed at improving patient safety and quality of care have also encouraged the adoption of DUM practices among healthcare providers and insurers. Moreover, the shift towards value-based care models has incentivized stakeholders to implement DUM strategies that enhance patient outcomes and satisfaction while containing costs. All these factors collectively contribute to the expansion and evolution of the U.S. Drug Utilization Management market.
What are the Key Trends in the U.S. Drug Utilization Management Market?
• Increased Adoption of Electronic Health Records: Healthcare providers all over the world are increasingly leveraging EHR systems in order to streamline DUM processes, including medication history tracking and decision support tools for prescribing.
• Value-Based Care Initiatives: There is a growing emphasis on DUM techniques that align with value-based care models, such as medication adherence programs and outcomes-based contracting.
• Advancements in Data Analytics: The increased use of big data and analytics enables healthcare organizations in analyzing prescribing patterns, identify potential misuse or overuse of medications as well as optimize treatment protocols with the help of predictive modeling.
• Integration of Artificial Intelligence and Machine Learning: AI and ML technologies are increasingly being integrated into DUM systems to enhance decision-making processes, personalize patient care pathways and predict medication efficacy in a more accurate manner.
• Rise in Specialty Medications: The increasing availability and utilization of specialty drugs facilitates more stringent DUM strategies in order to ensure appropriate use, manage cost, and coordinate care across healthcare settings.
Discover the Full Market Insights 👉
https://www.visionresearchreports.com/us-drug-utilization-management-market/41416
What are the Major Challenges in the U.S. Drug Utilization Management Market?
One of the major challenges which are hindering the growth and development of the U.S drug utilization management market is the administrative complexity that is imposed on healthcare providers and the potential delays they tend to create for patients. Drug utilization management has several requirements, such as prior authorizations that consume valuable clinical time and delay access to necessary medications.
In addition to that, the time-consuming nature of these processes can increase clinician burnout and also hamper the quality of patient-provider interactions. Manual documentation, long waiting times for payer approvals and the lack of interoperability among health IT systems further amplifies the problem. These drawbacks can lead to decreased adherence, worsened health outcomes or even unnecessary emergency room visits. These limitations in turn slow down-market entry and potential.
What are the Key Opportunities in the U.S. Drug Utilization Management Market?
The increased integration of artificial intelligence and drug utilization management presents various growth opportunities in the U.S. market. AI technologies, especially natural language processing (NLP) and machine learning (ML) models have proved to have great potential in streamlining and optimizing DUM processes. AI tools can now be trained in order to evaluate clinical documentation, detect incomplete authorizations, identify patient-specific drug risks and even recommend alternative therapies with much greater speed and accuracy than compared to traditional manual reviews.
Several tech-driven startups and vendors all over the world have already begun adopting AI-based platforms into their workflows, with aims to integrate them directly with electronic health records (EHRs) and pharmacy benefit management systems. These types of platforms can help reduce the administrative burden faced by healthcare providers, minimize errors, and even accelerate decision-making processes. As AI continues to make its mark in real-world deployments, it could completely reshape and revolutionize how drug utilization management will be carried out in the upcoming years.
U.S. Drug Utilization Management Market Report Coverage
|
Report Attribute |
Key Statistics |
|
Market Size in 2025 |
USD 42.81 Billion |
|
Market Size in 2026 |
USD 46.02 Billion |
|
Market Size in 2030 |
USD 61.45 Billion |
|
Market Size in 2032 |
USD 71.02 Billion |
|
Market Size by 2034 |
USD 82.07 Billion |
|
Growth rate from 2025 to 2034 |
CAGR of 7.5% |
|
Base Year |
2024 |
|
Forecast Period |
2025 to 2034 |
|
Segments Covered |
By Program Type, By End-use |
|
Companies Covered |
Prime Therapeutics LLC, MedicusRx, EmblemHealth, Optum Inc., Point32Health Inc., AssureCare LLC, MindRx Group, Agadia Systems Inc., Elevance Health (CarelonRx), ExlService Holdings Inc., MRIoA, S&C Technologies Inc., Ultimate Health Plans, Security Health Plan of Wisconsin Inc., Blue Cross and Blue Shield Association, Providence, Simply Healthcare Plans Inc. |
For Orders or Inquiries, Don’t Hesitate to Reach Out: sales@visionresearchreports.com
U.S. Drug Utilization Management Market Segmental Analysis
Program Type Analysis
Which Program Type Dominated the Market in 2024?
The in-house segment dominated the market in 2024. This segment's dominance is attributed to its ability to deliver cost savings, efficient utilization management and streamlined administrative processes for health plans and employers. Moreover, high utilization of prescription drugs in the region necessitates efficient in-house programs for handling prescription amounts filled by retail pharmacies.
The outsourced segment is expected to experience the fastest growth throughout the forecast period. The increasing demand for outsourced programs in the U.S. is primarily driven by healthcare provider’s emphasis on delivering high-quality care alongside efficient utilization management services. This approach aims to optimize patient care while effectively managing healthcare costs, thus fueling the growth of this segment.
End-use Analysis
Which End User Held the Largest Market Share in 2024?
The PBMs segment held the largest market share in 2024. This is because they play a very important role in negotiating discounted drug prices and securing refunds from pharmaceutical manufacturers. Through effective management of drug formularies and utilization, PBMs help to mitigate medication costs for health insurance plans and employers. They also help to streamline operations by overseeing administrative tasks such as pharmacy network management, claims processing, and benefit plan design, which in turn, lessens the workload for insurers, employers and pharmacies.
The health plan provider/payors segment is seen to have the fastest growth rate during the forecast period. Stakeholders in the region are increasingly focused on addressing factors that are contributing to high costs. Health plan providers leverage drug utilization management strategies to curtail unnecessary services and ensure patients receive appropriate, high-quality and cost-effective care. This strategic and patient centric approach is likely to drive the growth of this segment.
Need a Tailored Version of the Report? | Get Customization Options Here: https://www.visionresearchreports.com/report/customization/41416
Recent Developments in the U.S. Drug Utilization Management Market
• In November 2025, CMS announced the generating cost Reductions for U.S. Medicaid (GENEROUS) Model, a new drug payment model that will aim to lower prescription drug spending in Medicaid and strengthen the program overall. The GENEROUS model, launching in 2026, will allow participating states to purchase drugs included in the pilot at prices in line with those in other nations, with a goal of increasing access to medications and improving health outcomes among Medicaid beneficiaries.
• In October 2025, Trump announced a landmark deal with Pfizer granting the company a three-year reprieve from planned tariffs in exchange for voluntarily lowering US drug prices. Pfizer will offer most-favored-nation pricing for Medicaid and all new drugs, participate in the TrumpRx direct-to-consumer platform. Under the deal, Pfizer will provide Medicaid with most-favored-nation pricing. The agreement also ensures that this pricing model will apply to all new drugs launched in the US.
Browse More Insights:
• Local Anesthesia Drugs Market: https://www.visionresearchreports.com/local-anesthesia-drugs-market/41721
• Ultomiris Drug Market: https://www.visionresearchreports.com/ultomiris-drug-market/41718
• Antifungal Drugs Market: https://www.visionresearchreports.com/antifungal-drugs-market/41717
• Contraceptive Drugs and Devices Market: https://www.visionresearchreports.com/contraceptive-drugs-and-devices-market/41596
• Antibody Drug Conjugates Market: https://www.visionresearchreports.com/antibody-drug-conjugates-market/41295
• Generic Drugs Market: https://www.visionresearchreports.com/generic-drugs-market/41283
• U.S. Generic Drugs Market: https://www.visionresearchreports.com/us-generic-drugs-market/41282
• Morphine Drugs Market: https://www.visionresearchreports.com/morphine-drugs-market/41174
• Drug Discovery Market: https://www.visionresearchreports.com/drug-discovery-market/41160
• North America Topical Drugs CDMO Market: https://www.visionresearchreports.com/north-america-topical-drugs-cdmo-market/41155
• Psychedelic Drugs Market: https://www.visionresearchreports.com/psychedelic-drugs-market/41096
• Anti-hypertensive Drugs Market: https://www.visionresearchreports.com/anti-hypertensive-drugs-market/41039
• Antiemetics Drugs Market: https://www.visionresearchreports.com/antiemetics-drugs-market/41038
Top Key Players in the U.S. Drug Utilization Management Market
• Optum, Inc.
• Point32Health, Inc.
• AssureCare LLC
• MindRx Group
• Agadia Systems, Inc
• Elevance Health (Carel
• Ultimate Health Plans
• Security Health Plan of Wisconsin, Inc.
• Blue Cross and Blue Shield Association
• Providence
• Simply Healthcare Plans, Inc
• Health Plan of San Mateo (HPSM)
• PerformRx
• Aetna, Inc. (CVS Health Corp.)
Segments Covered in the Report
By Program Type
• In-house
• Outsourced
By End-use
• PBMs
• Health Plan Provider/Payors
• Pharmacies
Instant Delivery Available | Purchase This Exclusive Research Report Now: https://www.visionresearchreports.com/report/checkout/41416
You can place an order or ask any questions, please feel free to contact at: sales@visionresearchreports.com
About Us
Vision Research Reports is a premier service provider offering strategic market insights and solutions that go beyond traditional surveys. We specialize in actionable market research, delivering in-depth qualitative insights and strategies to global industry leaders and executives, helping them navigate future uncertainties. Our offerings include consulting services, syndicated market studies, and bespoke research reports.
We are committed to excellence in qualitative market research, fostering a team of experts with deep industry knowledge. Our goal is to help clients understand both current and future market trends, empowering them to expand their portfolios and achieve their business objectives with the right guidance.
Web: https://www.visionresearchreports.com
Our Trusted Data Partners
Precedence Research | Statifacts | Nova One Advisor
For Latest Update Follow Us: LinkedIn
Discover More Market Trends and Insights from Vision Research Reports:
• Kidney Preservation Market: https://www.visionresearchreports.com/kidney-preservation-market/41699
• Virus Filtration Market: https://www.visionresearchreports.com/Virus-filtration-market/41685
• Tele-consulting Services Market: https://www.visionresearchreports.com/tele-consulting-services-market/41680
• Practice Management System Market: https://www.visionresearchreports.com/practice-management-system-market/41679
• Gene Therapy Platform Market: https://www.visionresearchreports.com/gene-therapy-platform-market/41678
• Infectious Disease In Vitro Diagnostics Market: https://www.visionresearchreports.com/infectious-disease-in-vitro-diagnostics-market/41672
• AI In Revenue Cycle Management Market: https://www.visionresearchreports.com/ai-in-revenue-cycle-management-market/41664
• Agricultural Biotechnology Market: https://www.visionresearchreports.com/agricultural-biotechnology-market/41665
• Bioconjugation Market: https://www.visionresearchreports.com/bioconjugation-market/41666
• Bioinformatics Services Market: https://www.visionresearchreports.com/bioinformatics-services-market/41669
• Personalized Cancer Vaccine Market: https://www.visionresearchreports.com/personalized-cancer-vaccine-market/41670

