Use of outpatient mental health services up nearly 20%, anxiety and depression top list of telehealth diagnoses Spending on substance use disorder treatment increased 10%
|
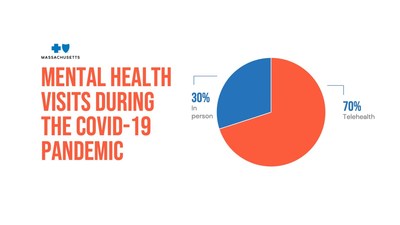
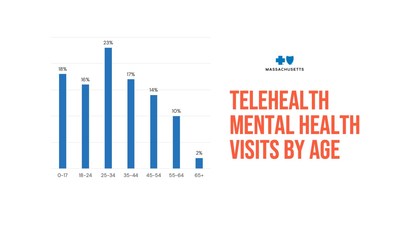
BOSTON, May 6, 2021 /PRNewswire/ -- Use of outpatient mental health services, including psychotherapy, increased nearly 20% during the COVID-19 crisis, and spending on substance use disorder treatment increased by 10%, according to data released today by Blue Cross Blue Shield of Massachusetts ("Blue Cross"). Nearly three quarters of members' mental health visits during the pandemic have been conducted via telehealth, either via phone or virtually, and 60% of mental health diagnoses made via telehealth have been for anxiety.
"Unlike medical services, which were largely deferred during the first several months of the pandemic, mental health claims have increased significantly," said Dr. Ken Duckworth, senior medical director for behavioral health at Blue Cross. "Kids, teens, adults – we're seeing unprecedented demand for care. The good news is that our members are getting help – both in-person and virtually." Mental health care via telehealth "This has been a transformation in care delivery unlike anything I've ever seen," noted Dr. Duckworth. "We're going to see sustained interest in telehealth for mental health care, even after the pandemic subsides. Many members tell us they appreciate the convenience and added flexibility virtual care offers, and clinicians report fewer missed or cancelled appointments. While there are obviously some exceptions, the feedback we've heard from patients and practitioners has been largely positive." Substance use disorder "The entire addiction treatment field was disrupted almost overnight," said Dr. Gregory Harris, senior medical director for behavioral health at Blue Cross. "The pandemic affected every aspect of substance use disorder care, but fortunately, we were able to work with clinicians to find creative solutions. Telehealth allowed many members to continue to get the SUD treatment they needed, even for higher levels of care like intensive outpatient and partial hospitalization programs." Blue Cross took several steps to improve members' access to SUD services via telehealth during the pandemic, including allowing visits to be conducted via both video and phone, since telephonic visits may be particularly useful for members who do not have internet access or privacy. More members using online tools to improve mental health Participation has exceeded expectations with more than 1,000 members per month enrolling in the program. 60% of these members had not previously been in therapy for these conditions. Blue Cross members using Learn to Live to address depression or stress, anxiety and worry report an average improvement of 30%. Connecting members with the right care Blue Cross members who need assistance finding mental health and/or substance use disorder services can visit the company's mental health resource center or call the number on their member ID card. Blue Cross representatives can help locate appropriate clinicians who are accepting new patients and even assist with setting up the first visit. About Blue Cross Blue Shield of Massachusetts
SOURCE Blue Cross Blue Shield of Massachusetts |
||||||||||||||||||