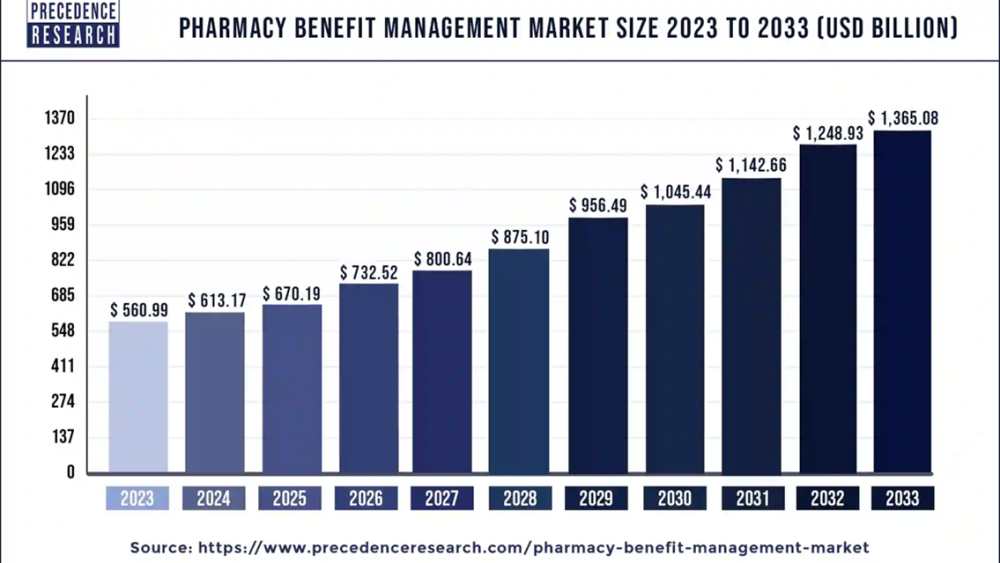
The global pharmacy benefit management market was evaluated at US$ 560.99 billion in 2023 and is expected to attain around US$ 1,365.08 billion by 2033, growing at a CAGR of 9.3% from 2024 to 2033.
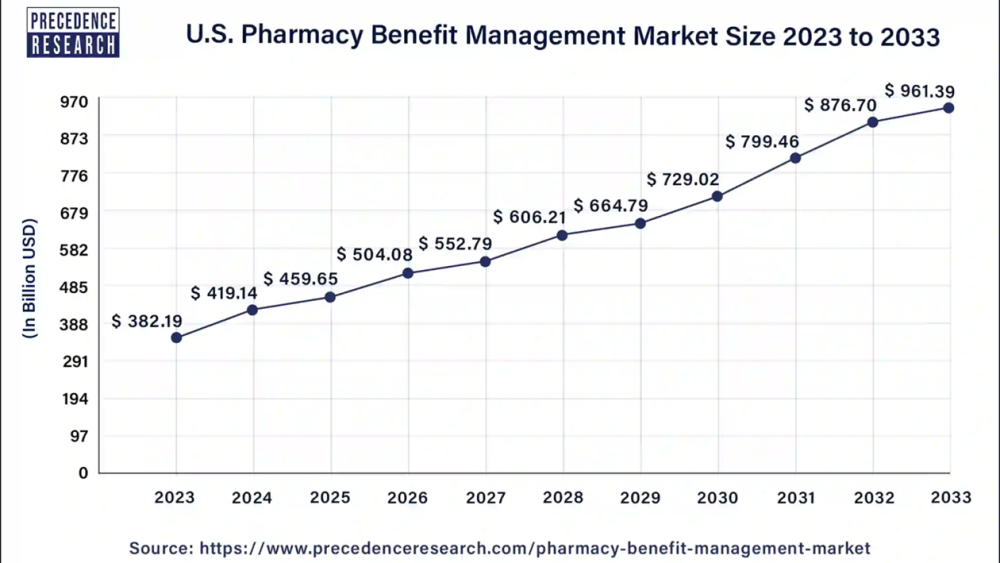
The U.S. pharmacy benefit management market size was valued at USD 382.19 billion in 2023 and is expected to reach around USD 961.39 billion by 2033 with a CAGR of 9.7% from 2024 to 2033.
The burgeoning market for pharmacy benefit management (PBM) is significantly driven by their pivotal role in managing prescription drug benefits for health insurers, Medicare Part D plans, large employers, and other payers.
Ask here for sample copy of report@ https://www.precedenceresearch.com/sample/1770
Pharmacy Benefit Management Market Overview
The pharmacy benefit management (PBM) industry is experiencing rapid growth, driven by its crucial role as intermediaries among insurance companies, pharmacies, and drug manufacturers. PBMs are tasked with securing lower drug costs for insurers by negotiating discounts with pharmacies and drug manufacturers, with savings passed on to insurance companies. Profits are generated through slight up-charging or retaining portions of rebates. As an integral part of the multilayered insurance industry, PBMs are pivotal in managing costs, negotiating discounts in exchange for promoting manufacturers’ drugs to a vast customer base, and establishing pharmacy networks for drug distribution.
The federal Centers for Medicare and Medicaid Services have highlighted PBMs' effectiveness in leveraging their negotiating power to lower drug prices and curb drug spending growth over recent years. The potential for PBMs to favor high-priced drugs over cost-effective alternatives presents a complex dynamic in the industry. This intricate balance of roles and incentives underscores the burgeoning demand for PBM services, fueling the market's expansion.
Key Insights
· North America has accounted highest market share of 97.14% in 2023.
· Asia Pacific region is poised to grow at a fastest CAGR between 2024 and 2033.
· By Service, the Specialty Pharmacy Services segment has accounted market share of 34% in 2023.
· By Service Provider, the insurance companies segment has generated highest revenue share in 2023.
Buy This Premium Research Report@ https://www.precedenceresearch.com/checkout/1770
Regional Stance
North America commands a dominant position in the global pharmacy benefit management (PBM) market, with key players such as Express Scripts Canada (ESC) and Telus Health leading the industry in Canada. It is estimated that these two entities handle 80% of all private drug claims for major companies like Sun Life, Canada Life, and Manulife. Additional Canadian PBMs include Canada Life’s ClaimSecure, Green Shield Canada’s HBM+, and Blue Cross Canada’s PBM. In the United States, PBMs face intense scrutiny due to practices of receiving rebates from manufacturers, which can lead to artificially inflated drug costs for patients. This scrutiny has highlighted instances where pharmacies incur losses on prescriptions they dispense, adding complexity to the regulatory landscape and operational challenges within the PBM market.
· In February 2024, Better Therapeutics signed a rebate agreement with one of the largest pharmacy benefit managers in the US for its AspyreRx diabetes treatment.
The Asia Pacific region is poised for significant growth in the pharmacy benefit management market during the forecast period. In India, the government has implemented national and state-specific healthcare policies targeting the lower-income class, which is expected to drive the demand for PBM services. The healthcare industry's susceptibility to annual inflation has led insurance providers to increase premiums for their policy offerings, further amplifying the need for efficient cost management solutions provided by PBMs. This dynamic, coupled with a growing emphasis on accessible healthcare, positions Asia Pacific as a critical region for the expansion of the pharmacy benefit management market.
Request here for custom research report@ https://www.precedenceresearch.com/customization/1770
Report Highlights
By Services
The specialty pharmacy segment has emerged as the largest revenue contributor within the pharmacy benefit management market, driven by its vital role in streamlining delivery processes and addressing healthcare delivery and financing challenges for providers and insurers. The growing significance of specialty pharmacies (SP) is directly linked to the evolving financial and third-party payment complexities that healthcare organizations encounter. By offering tailored services that enhance efficiency and mitigate these challenges, SPs have solidified their position as an indispensable component of the PBM landscape, driving substantial revenue growth in this segment.
The benefit plan design and administration segment is projected to be the most opportunistic within the pharmacy benefit management market during the forecast period. This segment encompasses the creation, management, and updating of an organization’s employee benefits program, which is crucial for long-term business success. A robust benefits strategy not only enhances employee satisfaction and retention but also ensures compliance with legal requirements mandating certain benefits for eligible employees. As companies increasingly recognize the strategic importance of comprehensive benefits administration, this segment is poised for substantial growth, offering significant opportunities within the pharmacy benefit management market.
By Service Provider
The insurance companies segment has emerged as the dominant service provider segment in the global pharmacy benefit management market. These companies depend heavily on PBMs to manage and control prescription drug costs, positioning PBMs as crucial intermediaries. By negotiating substantial discounts with drug manufacturers, PBMs ensure that insurers can offer competitive drug prices to their policyholders while promoting the manufacturers' drugs to a broad customer base. PBMs establish extensive retail pharmacy networks through strategic contracts, facilitating efficient drug distribution. This intermediary role underscores the significant influence of insurance companies within the pharmacy benefit management market, driving its continued growth and evolution.
The retail pharmacy segment, also known as community pharmacy, is projected to be the fastest-growing segment in the pharmacy benefit management (PBM) market during the forecast period. Easily accessible within local communities, these pharmacies provide essential medications and offer valuable advice to ensure safe and effective medication use. Traditionally referred to as chemist or pharmacist shops, retail pharmacies play a critical role in educating customers about drug interactions, including interactions with alcohol, and preventing problematic medication combinations. This accessibility and direct customer interaction underscore the segment's rapid growth potential, driven by the increasing demand for convenient and informed pharmaceutical care.
Related Reports
· U.S. Pharmacy Benefit Management Market: https://www.precedenceresearch.com/us-pharmacy-benefit-management-market
· Pharmacy Automation Market: https://www.precedenceresearch.com/pharmacy-automation-market
· Pharmacy Management System Market: https://www.precedenceresearch.com/pharmacy-management-system-market
· Pharmacy Automation Devices Market: https://www.precedenceresearch.com/pharmacy-automation-device-market
Market Dynamics
Driver
PBMs' Expanding Role and Increased Scrutiny
Pharmacy benefit managers (PBMs) have significantly expanded their influence within the pharmaceutical supply chain by acting as intermediaries between pharmacies, plan sponsors, pharmaceutical manufacturers, and drug wholesalers. Their responsibilities now encompass claims processing, formulary management, pharmacy networks, mail order pharmacies, and contracting with wholesalers and manufacturers. This expansion has enhanced their role and visibility, attracting increased scrutiny from policymakers. The heightened focus on PBMs' practices and their critical position in the supply chain has, in turn, driven growth in the pharmacy benefit management market, underscoring their essential function in modern healthcare.
Restraint
Lack of Transparency in PBM Operations
A significant challenge in demanding greater accountability from pharmacy benefit managers (PBMs) is the relative lack of transparency in their operations. The already opaque drug pricing process is further complicated by the additional layer of secrecy introduced by PBMs. Most insurers rely on PBMs to manage the administrative aspects of their drug benefit programs, yet PBMs are not obligated to disclose critical details to insurers. This includes how formulary placements are determined, why certain drugs are more expensive than others, and the proportion of rebates and negotiated drug payments retained by PBMs. This opacity hinders the growth of the pharmacy benefit management market by fostering uncertainty and limiting trust among stakeholders.
Opportunity
Expanding Role of PBMs in Disease Management
Pharmacy benefit managers (PBMs) are poised to play an increasingly vital role in the integrated management of patient care, particularly for high-cost chronic diseases and conditions. Their ability to reduce costs, provide national pharmacy access, and tailor benefits to diverse client needs in a highly automated environment underscores their potential for industry success. PBMs operate at scale with sophisticated automation to manage claims processing and deliver high-quality customer service. Their comprehensive service offerings span administrative functions such as benefit administration, pharmacy network management, and claims adjudication, as well as clinical services including formulary management and advanced utilization and disease management programs. This broad range of capabilities presents significant growth opportunities within the pharmacy benefit management market, positioning PBMs as pivotal players in optimizing healthcare outcomes and cost efficiencies.
Recent Developments
· In August 2023, David Blair launched a new pharmacy benefit management company.
· In May 2024, EmpiRx announced a new AI-powered platform as part of its initiative to transform PBMs.
Key Players in the Pharmacy Benefit Management Market
· CVS Health
· SS&C Technologies, Inc.
· Anthem Inc.
· Medimpact
· Express Scripts Holding Company
· Benecard Services, LLC
· CaptureRx Inc.
· Change Healthcare
· OptumRx, Inc.
Market Segmentation
By Service
· Specialty Pharmacy Services
· Benefit Plan Design & Administration
· Formulary Management
· Pharmacy Claims Processing
· Others
By Service Provider
· Retail Pharmacies
· Insurance Companies
· Standalone Pharmacy Benefit Management Providers
By Business Model
· Government Health Programs
· Employer-sponsored Programs
· Health Insurance Management
By Geography
· North America
· Europe
· Asia Pacific
· Latin America
· Middle East & Africa (MEA)
Buy This Premium Research Report@ https://www.precedenceresearch.com/checkout/1770
Call: USA: +1 650 460 3308 | IND: +91 87933 22019 | Europe: +44 2080772818
Email: sales@precedenceresearch.com
The U.S. pharmacy benefit management market size was valued at USD 382.19 billion in 2023 and is expected to reach around USD 961.39 billion by 2033 with a CAGR of 9.7% from 2024 to 2033.
The burgeoning market for pharmacy benefit management (PBM) is significantly driven by their pivotal role in managing prescription drug benefits for health insurers, Medicare Part D plans, large employers, and other payers.
Ask here for sample copy of report@ https://www.precedenceresearch.com/sample/1770
Pharmacy Benefit Management Market Overview
The pharmacy benefit management (PBM) industry is experiencing rapid growth, driven by its crucial role as intermediaries among insurance companies, pharmacies, and drug manufacturers. PBMs are tasked with securing lower drug costs for insurers by negotiating discounts with pharmacies and drug manufacturers, with savings passed on to insurance companies. Profits are generated through slight up-charging or retaining portions of rebates. As an integral part of the multilayered insurance industry, PBMs are pivotal in managing costs, negotiating discounts in exchange for promoting manufacturers’ drugs to a vast customer base, and establishing pharmacy networks for drug distribution.
The federal Centers for Medicare and Medicaid Services have highlighted PBMs' effectiveness in leveraging their negotiating power to lower drug prices and curb drug spending growth over recent years. The potential for PBMs to favor high-priced drugs over cost-effective alternatives presents a complex dynamic in the industry. This intricate balance of roles and incentives underscores the burgeoning demand for PBM services, fueling the market's expansion.
Key Insights
· North America has accounted highest market share of 97.14% in 2023.
· Asia Pacific region is poised to grow at a fastest CAGR between 2024 and 2033.
· By Service, the Specialty Pharmacy Services segment has accounted market share of 34% in 2023.
· By Service Provider, the insurance companies segment has generated highest revenue share in 2023.
Buy This Premium Research Report@ https://www.precedenceresearch.com/checkout/1770
Regional Stance
North America commands a dominant position in the global pharmacy benefit management (PBM) market, with key players such as Express Scripts Canada (ESC) and Telus Health leading the industry in Canada. It is estimated that these two entities handle 80% of all private drug claims for major companies like Sun Life, Canada Life, and Manulife. Additional Canadian PBMs include Canada Life’s ClaimSecure, Green Shield Canada’s HBM+, and Blue Cross Canada’s PBM. In the United States, PBMs face intense scrutiny due to practices of receiving rebates from manufacturers, which can lead to artificially inflated drug costs for patients. This scrutiny has highlighted instances where pharmacies incur losses on prescriptions they dispense, adding complexity to the regulatory landscape and operational challenges within the PBM market.
· In February 2024, Better Therapeutics signed a rebate agreement with one of the largest pharmacy benefit managers in the US for its AspyreRx diabetes treatment.
The Asia Pacific region is poised for significant growth in the pharmacy benefit management market during the forecast period. In India, the government has implemented national and state-specific healthcare policies targeting the lower-income class, which is expected to drive the demand for PBM services. The healthcare industry's susceptibility to annual inflation has led insurance providers to increase premiums for their policy offerings, further amplifying the need for efficient cost management solutions provided by PBMs. This dynamic, coupled with a growing emphasis on accessible healthcare, positions Asia Pacific as a critical region for the expansion of the pharmacy benefit management market.
Request here for custom research report@ https://www.precedenceresearch.com/customization/1770
Report Highlights
By Services
The specialty pharmacy segment has emerged as the largest revenue contributor within the pharmacy benefit management market, driven by its vital role in streamlining delivery processes and addressing healthcare delivery and financing challenges for providers and insurers. The growing significance of specialty pharmacies (SP) is directly linked to the evolving financial and third-party payment complexities that healthcare organizations encounter. By offering tailored services that enhance efficiency and mitigate these challenges, SPs have solidified their position as an indispensable component of the PBM landscape, driving substantial revenue growth in this segment.
The benefit plan design and administration segment is projected to be the most opportunistic within the pharmacy benefit management market during the forecast period. This segment encompasses the creation, management, and updating of an organization’s employee benefits program, which is crucial for long-term business success. A robust benefits strategy not only enhances employee satisfaction and retention but also ensures compliance with legal requirements mandating certain benefits for eligible employees. As companies increasingly recognize the strategic importance of comprehensive benefits administration, this segment is poised for substantial growth, offering significant opportunities within the pharmacy benefit management market.
By Service Provider
The insurance companies segment has emerged as the dominant service provider segment in the global pharmacy benefit management market. These companies depend heavily on PBMs to manage and control prescription drug costs, positioning PBMs as crucial intermediaries. By negotiating substantial discounts with drug manufacturers, PBMs ensure that insurers can offer competitive drug prices to their policyholders while promoting the manufacturers' drugs to a broad customer base. PBMs establish extensive retail pharmacy networks through strategic contracts, facilitating efficient drug distribution. This intermediary role underscores the significant influence of insurance companies within the pharmacy benefit management market, driving its continued growth and evolution.
The retail pharmacy segment, also known as community pharmacy, is projected to be the fastest-growing segment in the pharmacy benefit management (PBM) market during the forecast period. Easily accessible within local communities, these pharmacies provide essential medications and offer valuable advice to ensure safe and effective medication use. Traditionally referred to as chemist or pharmacist shops, retail pharmacies play a critical role in educating customers about drug interactions, including interactions with alcohol, and preventing problematic medication combinations. This accessibility and direct customer interaction underscore the segment's rapid growth potential, driven by the increasing demand for convenient and informed pharmaceutical care.
Related Reports
· U.S. Pharmacy Benefit Management Market: https://www.precedenceresearch.com/us-pharmacy-benefit-management-market
· Pharmacy Automation Market: https://www.precedenceresearch.com/pharmacy-automation-market
· Pharmacy Management System Market: https://www.precedenceresearch.com/pharmacy-management-system-market
· Pharmacy Automation Devices Market: https://www.precedenceresearch.com/pharmacy-automation-device-market
Market Dynamics
Driver
PBMs' Expanding Role and Increased Scrutiny
Pharmacy benefit managers (PBMs) have significantly expanded their influence within the pharmaceutical supply chain by acting as intermediaries between pharmacies, plan sponsors, pharmaceutical manufacturers, and drug wholesalers. Their responsibilities now encompass claims processing, formulary management, pharmacy networks, mail order pharmacies, and contracting with wholesalers and manufacturers. This expansion has enhanced their role and visibility, attracting increased scrutiny from policymakers. The heightened focus on PBMs' practices and their critical position in the supply chain has, in turn, driven growth in the pharmacy benefit management market, underscoring their essential function in modern healthcare.
Restraint
Lack of Transparency in PBM Operations
A significant challenge in demanding greater accountability from pharmacy benefit managers (PBMs) is the relative lack of transparency in their operations. The already opaque drug pricing process is further complicated by the additional layer of secrecy introduced by PBMs. Most insurers rely on PBMs to manage the administrative aspects of their drug benefit programs, yet PBMs are not obligated to disclose critical details to insurers. This includes how formulary placements are determined, why certain drugs are more expensive than others, and the proportion of rebates and negotiated drug payments retained by PBMs. This opacity hinders the growth of the pharmacy benefit management market by fostering uncertainty and limiting trust among stakeholders.
Opportunity
Expanding Role of PBMs in Disease Management
Pharmacy benefit managers (PBMs) are poised to play an increasingly vital role in the integrated management of patient care, particularly for high-cost chronic diseases and conditions. Their ability to reduce costs, provide national pharmacy access, and tailor benefits to diverse client needs in a highly automated environment underscores their potential for industry success. PBMs operate at scale with sophisticated automation to manage claims processing and deliver high-quality customer service. Their comprehensive service offerings span administrative functions such as benefit administration, pharmacy network management, and claims adjudication, as well as clinical services including formulary management and advanced utilization and disease management programs. This broad range of capabilities presents significant growth opportunities within the pharmacy benefit management market, positioning PBMs as pivotal players in optimizing healthcare outcomes and cost efficiencies.
Recent Developments
· In August 2023, David Blair launched a new pharmacy benefit management company.
· In May 2024, EmpiRx announced a new AI-powered platform as part of its initiative to transform PBMs.
Key Players in the Pharmacy Benefit Management Market
· CVS Health
· SS&C Technologies, Inc.
· Anthem Inc.
· Medimpact
· Express Scripts Holding Company
· Benecard Services, LLC
· CaptureRx Inc.
· Change Healthcare
· OptumRx, Inc.
Market Segmentation
By Service
· Specialty Pharmacy Services
· Benefit Plan Design & Administration
· Formulary Management
· Pharmacy Claims Processing
· Others
By Service Provider
· Retail Pharmacies
· Insurance Companies
· Standalone Pharmacy Benefit Management Providers
By Business Model
· Government Health Programs
· Employer-sponsored Programs
· Health Insurance Management
By Geography
· North America
· Europe
· Asia Pacific
· Latin America
· Middle East & Africa (MEA)
Buy This Premium Research Report@ https://www.precedenceresearch.com/checkout/1770
Call: USA: +1 650 460 3308 | IND: +91 87933 22019 | Europe: +44 2080772818
Email: sales@precedenceresearch.com