IRA
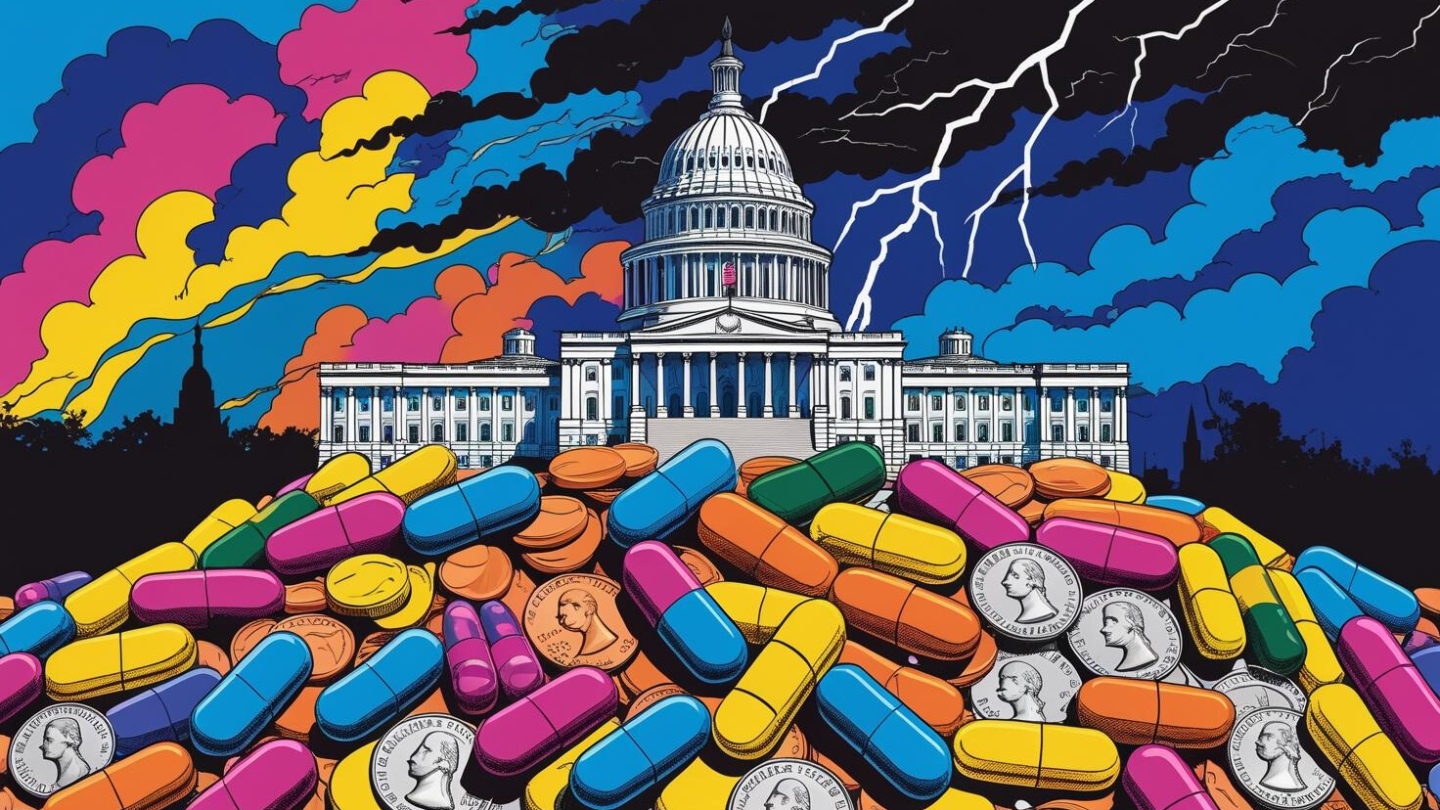
More than a dozen pharmas have recently struck deals with the White House to lower drug prices. Nevertheless, drugmakers reportedly plan to raise the U.S. prices of at least 350 branded medications.
Regulations aiming to lower the cost of vital medicines will instead end up restricting access and disincentivizing R&D.
The regulatory environment is placing extreme pricing pressure on pharmaceutical manufacturers. Their success in the market depends on mounting an agile response.
Under the Inflation Reduction Act, medications with the same active ingredient will be treated as the same drug for price negotiation purposes—even if approved by the FDA under a separate application—disincentivizing companies from investing time and money in gaining approval for new formulations and indications.
In advance of CMS’ negotiated price for the blood thinner taking effect next year, partners Bristol Myers Squibb and Pfizer pitched the direct-to-consumer program as a way to allow uninsured, underinsured and self-pay patients to pay less out of pocket.
Drug pricing, budget cuts, tariffs and other shifts under the Trump administration undermine the biopharma and healthcare ecosystem.
The new version of the bill will still need to go through the entire House and Senate.
The overturning of the FDA’s lab-developed tests rule is just the tip of the iceberg. With the loss of Chevron deference, power has shifted from federal agencies to the courts, with potential implications for everything from the FDA shortage list to CMS drug price negotiations.
From a higher bar for regulatory clearance to pricing limitations, drug development is more expensive than ever. This has led firms to make tough pipeline decisions early in the development process. The result may be costly for all of us.
Merck’s Keytruda holds on to the top spot while AbbVie’s Humira—once the world’s top-selling drug—continues to cede its market share to biosimilar competitors.